Private: Main Body
16 Contemporary Topics: Human Biology and Health
Joylin Namie, PhD, Truckee Meadows Community College
Learning Objectives
- Describe what is meant by a “mismatch” between our evolved biology and contemporary lifestyles and how this is reflected in modern disease patterns.
- Describe diet and physical activity patterns among preagricultural hunter-gatherers.
- Describe changes in subsistence, diet, and activity patterns that occurred as a result of the transition to food production and how these affected health among early agriculturalists.
- Explain what is meant by an epidemiological transition and describe the major transitions in patterns of disease among humans that have occurred throughout human evolution.
- Explain what is meant by examining health issues from an ecological perspective.
- Discuss examples of contemporary evolution.
When is the last time you needed to do research for an upcoming paper? I bet you started by looking for information online. How did you go about your search? Which websites looked promising? Which ones did not entice you to click past the home page? Once you found one you thought might be useful, how much time did you spend searching for information? At what point did you decide to leave that site and move on? I would wager money that you never once thought your behavior had anything do with human evolution, but it does.
Although we may not often stop to think about it, our evolutionary past is reflected in many aspects of modern life. The ways we “forage” for information on the internet mimics the ways we once foraged for food during our several-million-year history as hunter-gatherers (Chin et al. 2015). Humans are visual hunters (Lieberman 2006). We practice optimal foraging strategy, meaning we make decisions based on energy return for investment (McElroy and Townsend 2009). When we search for information online, we locate a “patch,” in this case a website or research article, then quickly scan the contents to discern how many resources it has that we can use. Like our hominin ancestors, we spend more time in “patches” with abundant resources and abandon sites quickly and move on once we have exhausted the available goods. As with internet searches, our evolutionary past is also reflected in the kinds of landscapes we find appealing, the foods that taste good to us, why we break a sweat at the gym, and why we have to go to the gym at all (Bogin 1991; Dutton 2009; Lieberman 2015). Many of the health problems facing humans in the 21st century also have their beginnings in the millions of years we roamed the earth as foragers.
This chapter addresses contemporary health issues from an evolutionary perspective. It begins with a review of diet, activity patterns, and causes of and among our preagricultural ancestors, which form the foundation for the ways our bodies function today. This is followed by a discussion of the health consequences of the transition to agriculture, marking the first of three major experienced by humankind. It then hones in on health conditions that have become all too familiar to those of us living in modern, industrialized societies, including , diabetes, heart disease, , , and the impact of stress on health. The environments in which we now live and the choices we make put a strain on biological systems that came about in response to selective pressures in our past. Furthermore, the transitions happened too quickly for natural selection to keep up (Stearns et al. 2008).
PREAGRICULTURAL HUMANS
Diet
Higher primates, including humans, may be the species with the longest list of nutritional requirements (Bogin 1991). This is likely due to the fact that we evolved in environments where there was a high diversity of species but low densities of any given species. Humans require 45–50 essential nutrients for growth, maintenance, and repair of cells and tissues. These include protein, carbohydrates, fats, vitamins, minerals, and water. As a species, we are (or were) highly active with high metabolic demands. Humans are not . We cannot manufacture our own nutrients. Doing so is metabolically expensive, meaning it takes a lot of energy to accomplish it. If the surrounding environment can provide those nutrients, it makes evolutionary sense to obtain them from outside the body, rather than spending energy producing them, as green plant species do (National Geographic Society n.d.). Given our nutritional requirements and caloric needs, it is not surprising that humans are and evolved to choose foods that are dense in essential nutrients. One of the ways we identified high-calorie resources in our evolutionary past was through taste, and it is no accident that humans find sweet, salty, fatty foods appealing.
The human predisposition toward sugar, salt, and fat is innate (Farb and Armelagos 1980). This is reflected in receptors for sweetness found in every one of the mouth’s ten thousand taste buds (Moss 2013). This tuning toward sweet makes sense in an ancestral environment where sweetness signaled high-value resources like ripe fruits. Likewise, “the long evolutionary path from sea-dwelling creatures to modern humans has given us salty body fluids, the exact salinity of which must be maintained” (Farb and Armelagos 1980), drawing us to salty-tasting things. Cravings for fat, another high-calorie resource, are also inborn, with some archaeological evidence suggesting that hominins may have been collecting bones for their fatty marrow, which contains two essential fatty acids necessary for brain development (Richards 2002), rather than for any meat remaining on the surface (Bogin 1991).
Archaeological and bone chemistry studies of preagricultural populations indicate that Paleolithic peoples ate a wider variety of foods than many people eat today (Armelagos et al. 2005; Bogin 1991; Larsen 2014; Marciniak and Perry 2017). Foragers took in more protein, less fat, much more fiber, and far less sodium than modern humans typically do (Eaton et al. 1988). Changes in tooth and intestinal morphology illustrate that animal products were an important part of human diets from the time of Homo erectus onward (Baltic and Boskovic 2015; Richards 2002; Wrangham 2009). These animal products consisted of raw meat scavenged from carnivore kills and marrow from the leftover bones. It is not possible to discern from current archaeological evidence when cooking began. The “cooking hypothesis” proposed by Richard Wrangham (2009) argues that H. erectus was adapted to a diet of cooked food, and phylogenetic studies comparing body mass, molar size, and other characteristics among nonhuman and human primates support this conclusion (Organ et al. 2011). However, the first documented archaeological evidence of human-controlled use of fire is dated to one million years ago, roughly a million years after the first appearance of H. erectus (Berna et al. 2012). Whenever cooking became established, it opened up a wider variety of both plant and animal resources to humans and led to selection for gene variants linked to reductions in the musculature of the jaw and thickness of tooth enamel (Lucock et al. 2014). However, the protein, carbohydrates, and fats preagricultural peoples ate were much different from those we eat today. Wild game, for example, lacked the antibiotics, growth hormones, and high levels of cholesterol and saturated fat associated with industrialized meat production today (Walker et al. 2005). It was also protein dense, providing only 50% of energy as fat (Lucock et al. 2014), and not prepared in ways that increase cancer risk, as modern meats often are (Baltic and Boskovic 2015).
Meats cooked well done over high heat and/or over an open flame, including hamburgers and barbecued meats, are highly carcinogenic due to compounds formed during the cooking process (Trafialek and Kolanowski 2014). Processed meats that have been preserved by smoking, curing, salting, or by adding chemical preservatives such as sodium nitrite (e.g., ham, bacon, pastrami, salami) have been linked to cancers of the colon, lung, and prostate (Abid et al. 2014) (See Figure 16.1). Nitrites/nitrates have additionally been linked to cancers of the ovaries, stomach, esophagus, bladder, pancreas, and thyroid (Abid et al. 2014). In addition, studies analyzing the diets of 103,000 Americans for up to 16 years indicate that those who ate grilled, broiled, or roasted meats more than 15 times per month were 17% more likely to develop high blood pressure than those who ate meat fewer than four times per month, and participants who preferred their meats well done were 15% more likely to suffer from than those who preferred their meats rare (Liu 2018). A previous study of the same cohort indicated “independent of consumption amount, open-flame and/or high-temperature cooking for both red meat and chicken is associated with an increased risk of Type 2 diabetes among adults who consume animal flesh regularly” (Liu et al. 2018). Although cooking, especially of meat (Wrangham 2009), has been argued to be crucial to cognitive and physical development among hominins, there has clearly been an evolutionary trade-off between the ability to preserve protein and the health risks humans experience due to consumption of cooked meat and exposure to chemical preservatives.

Although carbohydrates represent half of the diet on average for both ancient foragers and modern humans, the types of carbohydrates are very different. Ancient foragers ate fresh fruits, vegetables, grasses, legumes, and tubers, rather than the processed carbohydrates common in industrialized economies (Moss 2013). Their diets also lacked the refined white sugar and corn syrup found in many modern foods that, in themselves, contribute to the development of and diabetes (Pontzer et al. 2012).
Physical Activity Patterns
How do we know how active our ancestors really were? Hominin morphology and physiology provide us with clues. Consider our ancestral environment of sub-Saharan Africa. It was hot and dry, and close to the equator, meaning the sun was brighter and at a more direct angle than it is for many human populations today. This made the transition to bipedalism very important to survival. When the sun is at its highest in the sky, a bipedal human exposes only 7% of its surface area to maximal radiation, approximately one-third of the maximally exposed area of a similarly sized quadruped (Lieberman 2015). In a savannah environment where predators roamed in the cool of the night, it would have been evolutionarily advantageous for small, bipedal hominins to forage in the heat of the day, especially in an open habitat without the safety of trees. As early hominins were primarily scavengers who likely needed to travel to find food, heat-dissipating mechanisms would have been strongly favored.
Humans have four derived sets of adaptations for preventing hyperthermia (overheating): (1) fur loss and an increased ability to sweat (versus panting); (2) an external nose, allowing for nasal regulation of the temperature and humidity of air entering the lungs; (3) enhanced ability to cool the brain; and (4) an elongated, upright body. These adaptations suggest an evolutionary history of regular, strenuous physical activity. Some scholars have gone so far as to argue that, beginning with H. erectus, there are skeletal markers of adaptations for endurance running (Lieberman 2015; Richards 2002). The relevant morphological changes include modifications in the arches of the feet, a longer Achilles tendon, a nuchal ligament and ear canals that help maintain balance while running, shoulders decoupled from the head allowing rotation of the torso independently from the pelvis and head, and changes to the gluteus maximus. It is argued these modifications would have provided benefits for running, but not walking, and that H. erectus may have been running prey to the point of exhaustion before closing in for the kill (Lieberman 2015). This conclusion is controversial, with other scholars pointing to a lack of evidence for the necessary cognitive and projectile-making abilities among the genus Homo that far back in time (Pickering and Bunn 2007). Whether our ancestors were walking or running, they were definitely engaged in significant amounts of physical activity on a daily basis. They had to be or they would not have survived. As Robert Malina and Bertis Little (2008) point out, prolonged exertion and motor skills (e.g., muscular strength, tool making, and, eventually, accuracy with projectiles) are important determinants of success and survival in preindustrial societies.

Research with modern foraging populations, although controversial, can also offer clues to ancient activity patterns. Criticisms of such research include sampling bias due to the fact that modern foragers occupy marginal habitats and that such societies have been greatly influenced by their association with more powerful agricultural societies. Modern foragers may also represent an entirely new human niche that appeared only with climatic changes and faunal depletion at the end of the last major glaciation (Marlowe 2005). Despite these issues, the ethnographic record of foragers provides the only direct observations of human behavior in the absence of agriculture (Lee 2013). From such studies, we know hunter-gatherers cover greater distances in single-day foraging bouts than other living primates, and these treks require high levels of cardiovascular endurance (Raichlen and Alexander 2014). Recent research with the Hadza in Tanzania, one of the last remaining foraging populations, indicates that they walk up to 11 kilometers (6.8 miles) daily while hunting or in search of gathered foods (Pontzer et al. 2012), engaging in moderate-to-vigorous physical activity for over two hours each day—meeting the U.S. government’s weekly requirements for physical activity in just two days (Raichlen et al. 2016) (See Figure 16.2). The fact that humans were physically active in our evolutionary past is also supported by the fact that regular physical exercise has been shown to be protective against a variety of health conditions found in modern humans, including (Raichlen and Alexander 2014) and Alzheimer’s dementia (Mandsager et al. 2018), even in the presence of brain pathologies indicative of cognitive decline (Buchman et al. 2019).
Infectious Disease
Population size and density remained low throughout the Paleolithic, limiting morbidity and mortality from infectious diseases, which sometimes require large populations to sustain epidemics. Our earliest ancestors had primarily two types of infections to contend with (Armelagos 1990). The first were organisms that adapted to our prehominin ancestors and have been problems ever since. Examples include head lice, pinworms, and yaws. A second set of diseases were , diseases that originate in animals and mutate into a form infectious to humans. A contemporary example is the Human Immunodeficiency Virus (HIV) that originated in non-human primates and was likely passed to humans through the butchering of hunted primates for food (Sharp and Hahn 2011). Zoonoses that could have infected ancient hunter-gatherers include tetanus and transmitted by flies, mosquitoes, fleas, midges, and ticks. Many of these diseases are slow acting, chronic, or latent, meaning they can last for weeks, months, or even decades, causing low levels of sickness and allowing victims to infect others over long periods of time. Survival or cure does not result in lasting immunity with survivors returning to the pool of potential victims. Such diseases often survive in animal reservoirs, reinfecting humans again and again (Wolfe et al. 2012). A recent study of bloodsucking insects preserved in samples of amber dating from 15 to 100 million years ago indicate they carried microorganisms that today cause diseases such as filariasis, sleeping sickness, river blindness, typhus, Lyme disease, and malaria (Poinar 2018). Such diseases may have been infecting humans throughout our evolutionary history, and they may have had significant social and economic impacts on small foraging communities because they more often infected adults, who provided the food supply (Armelagos et al. 2005).
Health Profiles
Given their diets, levels of physical activity, and low population densities, the health profiles of preagricultural humans were likely better than those of many modern populations. This assertion is supported by comparative research conducted with modern foraging and industrialized populations. Measures of health taken from 20th-century foraging populations demonstrate excellent aerobic capacity, as measured by oxygen uptake during exertion, and low body-fat percentages, with triceps skinfold measurements half those of white Canadians and Americans. Serum cholesterol levels were also low, and markers for diabetes, hypertension, and cardiovascular disease were missing among them (Eaton et al. 1988; Raichlen et al. 2016). Life expectancies among our ancient ancestors are difficult to determine, but an analysis of living foragers by Michael Gurven and Hillard Kaplan (2007:331) proposed that, “for groups living without access to modern healthcare, public sanitation, immunizations, or an adequate or predictable food supply, at least one-fourth of the population is likely to live as grandparents for 15–20 years.” Based on their analysis, the maximum lifespan among our ancestors was likely seventy years of age, just two years less than average global life expectancy in 2016 (WHO 2018a).
HEALTH CONSEQUENCES OF THE TRANSITION TO AGRICULTURE AND ANIMAL DOMESTICATION
The shift from foraging to food production occurred relatively recently in our evolutionary history (Larsen 2014), and there are indications our biology has not yet caught up (Pritchard 2010). Beginning around 12,000 BCE in several parts of the globe, humans began to move to a diet based on domesticated plants and animals (Armelagos et al. 2005). This involved manipulating the natural landscape to facilitate intensive food production, including the clearing of forest and construction of wells, irrigation canals, and ditches, exposing humans to water-borne illnesses and parasites, and attracting mosquitos and other vectors of disease to human settlements. The heavy, repetitive physical labor of early agricultural production resulted in negative impacts on articular joints, including osteoarthritis (Larsen 2014). At the same time, nutritional diversity became restricted, focused on major cereal crops that continue to dominate agricultural production today, including corn, wheat, and rice (Jain 2012). This represented a major shift in diet from a wide variety of plant and animal foods to dependence on starchy carbohydrates, leading to increases in dental caries (cavities), reductions in stature and growth rates, and nutritional deficiencies (Larsen 2014). Domesticated animals added new foods to the human diet, including meat that was higher in fat and cholesterol than wild game as well as dairy products (Lucock et al. 2014). Agriculture provided the means to produce a storable surplus for the first time in human history, allowing some individuals to grow and consume more than others, leading to the beginnings of economic inequality (Harris 1989). Social hierarchies led to the unequal distribution of the basic resources for healthy living, concentrating infectious disease among the poor and malnourished (Zuckerman et al. 2014), a situation that continues to plague humanity today (Marmot 2005).
and a rise in population density accompanied the move to agriculture, increasing the risk of infectious disease. Agriculture often provided enough calories, if not enough nutrition, to increase fertility. That is, although diets were worse and people unhealthier, populations continued to grow, even in the midst of high levels of child and maternal mortality and short life expectancies (Omran 2005). Hygiene became an issue as large settlements increased the already-difficult problem of removing human wastes and providing uncontaminated water (Armelagos et al. 2005). Domesticated animals, including cattle, sheep, goats, pigs, chickens, and horses, provided reservoirs of zoonotic pathogens, which affected farmers more than foragers, as farmers were in closer proximity to their animals on a daily basis (Marciniak and Perry 2017). Many of these diseases became major killers of humankind, including influenza, tuberculosis, malaria, plague, syphilis, and smallpox, functioning as selective pressures in and of themselves (Cooling 2015). As these diseases encountered large human populations, malnourished and concentrated in early settlements, they caused major epidemics that traveled along newly established routes for trade, warfare, and colonization.
EPIDEMIOLOGICAL TRANSITIONS
Changes in diet and physical-activity patterns associated with agriculture, in conjunction with increased population densities and exposure to zoonoses, resulted in what is known as an epidemiological transition, a shift in the causes of morbidity and mortality among humankind (Omran 1971). The first epidemiological transition from foraging to food production resulted in increases in dental caries, nutritional deficiencies, infectious disease, and skeletal conditions like osteoarthritis, as well as decreases in growth and height (Larsen 2014). A second epidemiological transition occurred following the Industrial Revolution in Western Europe and the United States when socioeconomic, political, and cultural conditions contributed to improved standards of living, hygiene, and nutrition that minimized the effects of infectious disease, after which people began to experience the that are the focus of the remainder of this chapter (Omran 2005). With the addition of immunizations and other public health initiatives, modified forms of this transition remain ongoing in many low- and middle-income countries (Zuckerman et al. 2014), with several now facing a “” of disease, with poor, often rural, populations falling prey to infectious diseases, while more affluent citizens are victims of chronic illnesses. A third epidemiological transition is now underway as infectious diseases, some of them novel, others re-emergent, and others even multi-drug resistant, have once again become major health concerns (Harper and Armelagos 2010; Zuckerman et al. 2014). These include Ebola, HIV/AIDS, tuberculosis, malaria, dengue, Lyme disease, and West Nile virus, all zoonoses that initially spread to humans through contact with animals. These diseases are increasing their geographic ranges due to climate change, economic development, and deforestation (Baer and Singer 2009).
Patterns of morbidity and mortality continue to shift across the globe. As with the first epidemiological transition resulting from the adoption of large-scale agriculture, such shifts can be the direct, if unintended, result of human interactions with the environment. For example, there has been a well-documented rise in chronic inflammatory diseases (CIDs) in recent decades in developed countries (Versini et al. 2015). This includes increased rates of allergic conditions like asthma, as well as autoimmune diseases like rheumatoid arthritis, multiple sclerosis, Crohn’s disease, and inflammatory bowel disease. This has coincided with the decrease in infectious disease associated with the second epidemiological transition, and the two are related. The “hygiene hypothesis” postulates the rise in CIDs is a result of limited exposure to nonlethal environmental pathogens in utero and early childhood (Zuckerman and Armelagos 2014). Modern human societies have become so sanitized that we are no longer exposed to microorganisms that stimulate the development of a healthy immune system (Versini et al. 2015). “In effect, the lifestyle changes—sanitary improvements, pasteurization, use of antibiotics, and improved hygiene—that contributed to the second transition may have produced a substantial trade-off in health and quality of life, with developed nations exchanging a high burden of infectious disease for a higher burden of CIDs” (Zuckerman et al. 2014).
Similarly, the re-emergence of infectious disease, the third epidemiological transition, reflects the continuing relationship between humans, animals, and pathogens. Over 60% of between 1940 and 2004 have been of zoonotic origin, with over 70% stemming from human contact with wildlife (Jones et al. 2008). The global bushmeat trade currently devastating Africa’s wildlife is a continuing source of Ebola infection (Asher 2017), as well as the original source of HIV and viruses related to leukemia and lymphoma among humans (Zuckerman et al. 2014). Further, new strains of avian (bird) flu, some with mortality rates as high as 60% among human victims (WHO n.d.), are transmitted to humans through poultry production and contact with wild birds; these pose a looming global threat of epidemic disease (Davis 2005). Lastly, the use of antibiotics in commercial meat production is directly related to the rise of drug-resistant strains of previously controlled infectious diseases. An estimated 80% of antibiotics in the U.S. are used to promote growth and prevent infection in livestock, and drug-resistant bacteria from these animals are transmitted to humans through meat consumption (Ventola 2015).
These examples illustrate continuing interaction between humans, our evolved biology, and the physical and cultural environments in which we live. The remainder of this chapter will focus on selected noncommunicable diseases and the social, cultural, and environmental factors that contribute to their in modern, industrialized economies. We begin with the health condition that affects all of the others—obesity.
OBESITY
According to the World Health Organization (2017b), 1.9 billion of the world’s people are overweight and 650 million of these are obese. In the United States, 70% of Americans are overweight, and 40% of these meet the criteria for obesity. For the first time in human history, most of the world’s population lives in countries where overweight and obesity kill more people than hunger does (see Figure 16.3). Improvements in public health and food production have allowed a greater number of people to live past childhood and to have enough food to eat. This does not include everyone. Many people still struggle with poverty, hunger, and disease, even in the wealthiest of nations, including the United States. On a global scale, however, many people not only have enough food to survive but also to gain weight—and, notably, enough extra weight to cause significant health problems. Several aspects of life in modern, industrialized societies contribute to the obesity crisis.

Causes of Obesity
Although studies show differences in daily energy expenditure between modern foraging and farming populations in comparison with industrialized peoples, the major contributor to obesity in Western populations is energy intake (Pontzer et al. 2012). Many people not only eat too much but too much of the wrong things. Biological anthropologist Leslie Lieberman (2006) argues that contemporary humans continue to rely on cues from foraging strategies in our evolutionary past that are now counterproductive in the environments in which we now live.
Examine your own eating habits in the context of how humans once hunted and gathered. We relied on visual cues to find food, often traveling long distances to obtain it, then transporting it back to our home base. There we may have had to process it, by hand, to render it edible. Think of how much less energy it takes to find food now. If we have the financial resources, we can acquire big energy payoffs by simply sitting at home and using an app on our mobile phone to place an order for delivery. And, voila! High-calorie (if not highly nutritious) food arrives at our door within minutes. Should we venture out for food, search time is reduced by signage and advertising directing us toward high-density “patches” where food is available 24 hours a day. These include vending machines, gas stations, and fast-food outlets. Travel time is minimal and little human energy is used in the process (Lieberman 2006).
Foods are also prepackaged and prepared in ways that allow us to eat large quantities quickly. Think French fries or chicken nuggets, which we can easily eat with our hands while doing other things, like driving or watching television, rendering eating mindless and allowing us to take in food faster than our can let us know we are getting full. Modern “patches” offer low-fiber, calorie-dense resources, which allows us to eat larger quantities, a problem already encouraged by our larger portion sizes (Lieberman 2006). Processed foods are also engineered to appeal to hominin preferences for sweet tastes and fatty, creamy textures (Moss 2013). Remember from earlier chapters that natural selection favored depth perception, color vision, grasping hands, and coordinated eye-hand movements as general primate traits. Advertising and packaging now use our color vision against us, attracting us to products with little nutritional value and playing to our evolutionary predisposition toward variety. Remember those 50 different nutrients we require? That variety is now presented to us in the form of 55 different flavors of Oreo cookies (Cerón 2017), which we take out of the package and dip in milk using our hand-eye coordination and depth perception.
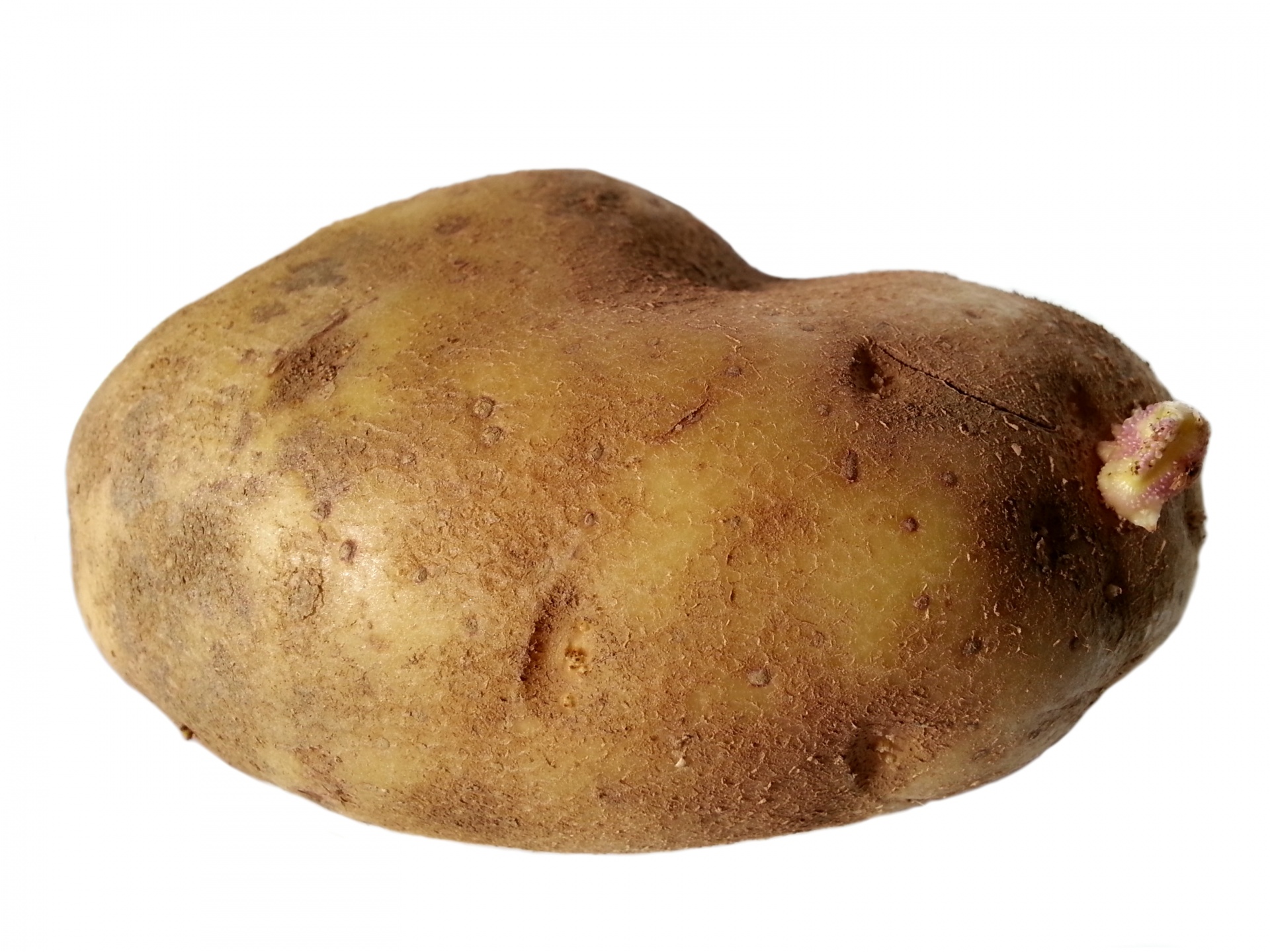
Even if we are ostensibly eating the same things our ancestors did, these foods may not be all that much alike. Take potatoes, for example. One medium-sized, plain, baked potato is a healthy food, especially if we eat the skin too. It contains 110 calories, 0 grams of fat, 26 grams of carbohydrates, and 3 grams of protein, plus 30% of the U.S. Recommended Daily Allowance (RDA) of vitamin C, 10% of vitamin B6, 15% of potassium, and no sodium (http://www.potatogoodness.com). In contrast, a medium order of McDonald’s fries, which takes the potato and adds salt and fat, contains 340 calories, 16 grams of fat, 44 grams of carbohydrates, 4 grams of protein, and 230 mg of sodium (http://www.mcdonalds.com). Potato chips take food processing to a whole new level, removing even more nutrition and adding a host of additional ingredients, including oils, preservatives, and artificial flavorings and colors (Moss 2013). Let us use Ruffles Loaded Bacon and Cheddar Potato Skins Potato Chips, one of the top new flavors of 2018, as an example (St. Pierre 2018). The number of ingredients increases from one to 11 to 35 as we move from the potato to the potato chip, moving further from nature with each step (Figure 16.4). It should be noted that the nutritional information for the potato chips is based on a serving size of 11 chips, an amount likely smaller than many people eat. Our bodies also do not react to fries and chips the same way they do to potatoes. Added fat and calories translate into overweight and obesity. Sodium contributes to hypertension. And, artificial flavorings and colorings, including the Yellow 5 and Yellow 6 in the chips, have been linked to cancer, as well as allergies and hyperactivity in children (CSPI 2010). Many sweet, fatty, salty foods like fries and chips are cheap and easily available, which is why many people choose to eat them (Moss 2013). The price of a medium-sized order of McDonald’s fries as of this writing is US$1.79, and the potato chips are $2.98 for an 8.5-ounce bag. A single potato prewrapped for microwaving is available in many supermarkets for US$1.99 but requires travel to a market and access to a microwave and eating utensils, making it less convenient.
Baked Potato [baked, skin on, plain] |

French Fries [medium order] |

Potato Chips [1 oz. serving of 11 chips] |
|
| Calories | 110 | 340 | 160 |
| Calories from fat | 0 | 144 | 90 |
| Fat | 0 g | 16 g | 10 g |
| Carbohydrates | 26 g | 44 g | 15 g |
| Protein | 3 g | 4 g | 2 g |
| Sodium | 0 g | 230 mg | 170 mg |
| Dietary fiber | 2 g | 4 g | 1 g |
| Sugars | 1 g | 0 g | 1 g |
| Cholesterol | 0 g | 0 g | 0 g |
| Ingredients | Potato | Potatoes, Vegetable Oil (Canola Oil, Soybean Oil, Hydrogenated Soybean Oil, Natural Beef Flavor [Wheat and Milk Derivatives]*, Citric Acid [Preservative]), Dextrose, Sodium Acid Pyrophosphate (Maintain Color), Salt. | Potatoes, Vegetable Oil (Sunflower, Corn, and/or Canola oil), Bacon & Cheddar Loaded Potato Skins Seasoning (Maltodextrin [Made from Corn], Salt, Cheddar Cheese [Milk, Cheese Cultures, Salt, Enzymes], Sour Cream [Cultured Cream, Skim Milk], Whey, Dried Onion, Monosodium Glutamate, Natural Flavor [including Natural Smoke Flavor], Skim Milk, Corn Oil, Canola Oil, Sugar, Buttermilk, Yeast Extract, Romano Cheese [Part-Skim Cow’s Milk, Cheese Cultures, Salt Enzymes], Whey Protein Concentrate, Dextrose, Spice, Citric Acid, Lactic Acid, Artificial Color [Yellow 5 Lake, Yellow 5, Yellow 6, Yellow 6 Lake], Butter [Cream, Salt], Sodium Caseinate, Garlic Powder, Blue Cheese [Milk, Cheese Cultures, Salt, Enzymes], and Bacon Fat. |
Figure 16.4 The potato in three modern forms.
Not only have we transformed the food supply and our eating in ways that are detrimental to our health, but these changes have been accompanied by reductions in physical activity. is built into contemporary lifestyles. Think of how much time you spent sitting down today. Some of it may have been in class or at work, some may have been driving a car or perhaps binge-watching your favorite show, playing a video game, or checking in on social media. An inactive lifestyle is almost dictated by the digital age (Lucock et al. 2014). Levels of physical activity in many countries are now so low that large portions of the population are completely sedentary, including 28% of Americans (Physical Activity Council 2018). For a species whose biology evolved in an environment where walking, lifting, and carrying were part of daily life, this is unhealthy and often leads to weight gain.
Obesity varies by gender, age, geography, and, to some degree, ethnicity (Brown 1991). In general, women tend to gain weight easier than men, but fat distribution is different between them. Women tend to put on weight in the thighs and hips, while men gain weight around their abdomen. The latter is a much greater health risk (Akil and Ahmad 2011). Weight gain also varies across the lifespan, with infants and toddlers tending toward chubbiness then becoming slimmer until adolescence and the onset of puberty (Lucock et al. 2014). This pattern is the result of selective pressure to maintain energy for brain development in early life, then again later on for reproduction. There is also the “thrifty gene” hypothesis: the idea that natural selection favored genotypes that clung to every calorie available to protect against the constant threat of food shortages throughout our evolutionary history, and that this was a species-wide adaptation (Neel 1962).

More recent genetic research indicates there are multiple genetic variants that influence weight gain, and they are not spread evenly across or within human populations. Tuomo Rankinen and colleagues (2006) identified 127 genes associated with obesity, of which 22 were supported by research indicating that they contributed to positive energy balance and weight gain. Claude Bouchard (2007) went further, identifying five categories of obesity-promoting genotypes. These include genotypes that promote sedentarism, result in low metabolism, and lead to poor regulation of appetite and satiety and a propensity to overeat. An example of the impact such genotypes can have in an environment of plenty is found among the population of the Micronesian island of Nauru. Historically, the island was geographically isolated and the food supply was unpredictable. These conditions favored genotypes that promoted the ability to rapidly build up and store fat in times of food availability. In Nauruans, there are two genetic variations favoring weight gain and insulin resistance, and both are associated with obesity and Type 2 diabetes. One variant is also associated with higher diastolic blood pressure. One of these variants is also found in Pima Indians in the United States, where it is associated with a high and Type 2 diabetes, although it is not associated with the same outcomes in Japanese and British subjects (de Silva et al. 1999). The other variant was also analyzed in Finnish and South Indian populations, neither of whom experienced the same outcome as Nauruans. This suggests these alleles may act as modifying genes for Type 2 diabetes in some population groups (Baker et al. 1994). Unfortunately, Nauruans are one of those groups. Eventually, they became wealthy through phosphate mining on the island, gaining access to a calorie-rich Western diet of imported foods and developing a sedentary lifestyle. This resulted in rates of Type 2 diabetes as high as 30–40% of Nauruans over the age of 15, which became the leading cause of death (Lucock et al. 2014), something Nauruans are taking seriously (See Figure 16.5).
Factors other than biology influence which populations carry and express a genetic predisposition toward obesity and which populations carry but do not express it. The Pima Indians, for example, were seriously impacted by U.S. government policies that affected water rights, forcing the population away from subsistence farming to dependence on government commodities and convenience food. This resulted in a significant loss of physical activity and sedentarism, as well as malnutrition and obesity. Those living on the reservation continue to experience hardship due to high rates of unemployment and poverty, as well as depression, sometimes made worse by alcoholism. In the absence of these pressures, the Pima were diabetes free for centuries prior, even though they relied on agriculture for subsistence, suggesting genetics alone is not responsible for high rates of obesity and diabetes in current populations (Smith-Morris 2004).
Obesity also has an epigenetic component. You learned about epigenetics in Chapter 3. With regard to obesity, epigenetics is counterintuitive in that mothers who do not take in enough calories during pregnancy often give birth to babies who grow up to be fat. What takes place is that the fetus receives signals from the mother through the placenta and intrauterine environment about environmental conditions during pregnancy, in this case food insecurity. These signals encourage the turning on and off of genes related to metabolism, for example. This alters the phenotype of the fetus so that if the child is born into an environment where food is readily available, it will put on weight rapidly whenever possible, falling prey to obesity and related diseases later in life. What is worse is that if the child is a girl, her own eggs are formed in utero with the same genetic changes coded in, meaning she will pass along this same genetic predisposition to gain weight to her children. Hence, a biological propensity toward obesity can continue across generations (Worthman and Kuzara 2005). This same mechanism operates in populations born into poverty that are now growing into plenty. Epigenetic changes to genes that promote weight gain are argued to be partly responsible for the rapid rise in obesity and diabetes in recent years in developing countries gaining access to Western diets (Stearns et al. 2008).
Obesity and overweight put a tremendous strain on several biological systems of the body, including the circulatory, endocrine, and skeletal systems, contributing to hypertension, heart disease, , diabetes, and osteoarthritis (See Figure 16.6). Obesity also elevates the risk of cancers of the breast, endometrium, kidney, colon, esophagus, stomach, pancreas, and gallbladder (National Institutes of Health 2017; Vucenik and Stains 2012). Diabetes, one of the fastest growing health conditions around the globe (WHO 2016) and one tightly connected to obesity and overweight, is the focus of the following Special Topics feature.

SPECIAL TOPIC: DIABETES

is an endocrine disorder characterized by excessively high blood glucose levels (Martini et al. 2013). According to a report released by the World Health Organization, the number of people living with diabetes is growing in all regions of the world. Rates of diabetes have nearly doubled in the past three decades, largely due to increases in obesity and sugary diets (WHO 2016). One in 11 people around the world, 435 million people, now have diabetes, including over 30 million Americans. In the United States, the disease is rising fastest among millennials (those ages 20-40) (BCBSA 2017), and one in every two adults with diabetes is undiagnosed (IDF 2018). Obesity and diabetes are linked: that is, obesity causes a diet-related disease (diabetes) because of humans’ evolved metabolic homeostasis mechanism, which is mismatched to contemporary energy environments (Lucock et al. 2014).
To function properly, cells need a steady fuel supply. Blood sugar is the primary fuel for most cells in the body, and the body produces the hormone to help move energy into cells that need it. Insulin functions like a key, turning on insulin receptors located on the surface of the cell. The receptor then activates glucose transporters (GLUTs) that do the work of hauling glucose (blood sugar) out of your bloodstream and into your cells (McKee and McKee 2015; see Figure 16.7). Foods that most readily supply glucose to your bloodstream are carbohydrates, especially starchy foods like potatoes or sweet, sugary foods like candy and soda. The body can also convert other types of foods, including protein-rich foods (e.g., lean meats) and fatty foods (e.g., vegetable oils and butter), into blood sugar in the liver via gluconeogenesis. Insulin’s main job is to tell your cells when to take up glucose. The cell also has to listen to the signal and mobilize the glucose transporters. This not only allows your cells to get the energy they need, but it also keeps blood sugar from building up to dangerously high levels when you are at rest. Muscles can use glucose without insulin when you are exercising; it does not matter if you are insulin resistant or if you do not make enough insulin. When you exercise, your muscles get the glucose they need, and, in turn, your blood glucose level goes down. If you are insulin resistant, resistance goes down when you exercise and your cells use glucose more effectively (Leontis n.d.).
This system is efficient, but there are limits. Keep in mind that, like the rest of our biology, it evolved during several million years when sugar was hard to come by and carbohydrates took the form of fresh foods with a low . Our ancestors were also active throughout the day, taking pressure off of the endocrine system. Now, sedentary lifestyles and processed-food diets cause many of us to take in more calories—and especially more carbohydrates—than our bodies can handle. The fact is, there is only so much blood sugar your cells can absorb. As soaring rates of diabetes show, many modern populations are taxing those limits. After years of being asked by insulin to take in more glucose than they can use, cells eventually stop responding (McKee and McKee 2015). This is called Type 2 diabetes or insulin resistance, which accounts for 90–95% of diabetes cases in the United States. People with Type 1 diabetes do not produce insulin (O’Keefe Osborn 2017; see Figure 16.8).

Type 2 diabetes is a progressive metabolic condition that occurs over time when our evolved biological mechanism that turns food into energy is derailed by the obesogenic environments in which we live. This is compounded by a sedentary lifestyle. Think about how living in a college environment contributes to the development of diabetes. How much time do you spend sitting each day? How many sugary—and often cheap—carbohydrates are within easy reach? Making simple changes now can head off health complications later. Carrying an apple or orange in your backpack instead of a candy bar and walking or biking instead of driving can make a big difference.
CARDIOVASCULAR DISEASE
Cardiovascular disease (CVD)—which includes coronary heart disease, hypertension (high blood pressure), and stroke—is the leading cause of death globally, and heart disease remains the number one cause of death in the United States (American Heart Association 2018). Risk factors for cardiovascular disease include diet, obesity/overweight, diabetes, and physical inactivity, as well as smoking and alcohol consumption. The connections between these factors and heart disease may not seem obvious and will be addressed here beginning with diet. Diets high in saturated fat and cholesterol can lead to atherosclerosis, a condition in which fat and cholesterol form plaque inside the arteries, eventually building up and hardening to the point that blood flow is blocked. Too much salt in the diet leads to fluid retention, which increases blood volume and thereby blood pressure, taxing the heart. Obesity/overweight contribute to cardiovascular disease directly through increases in total blood volume, cardiac output, and cardiac workload. In other words, the heart has to work much harder if one is overweight (Akil and Ahmad 2011).
Obesity also relates to CVD indirectly through elevation of blood pressure (hypertension) and diabetes. High levels of blood glucose from diabetes can damage blood vessels and the nerves that control the heart and blood vessels. Physical activity also alters the likelihood of having heart disease, both directly and indirectly. Regular exercise of moderate to vigorous intensity strengthens the heart muscle and allows capillaries, tiny blood vessels in your body, to widen, improving blood flow. Regular exercise can also lower blood pressure and cholesterol levels and manage blood sugar levels, all of which reduce the risk of CVD. Alcohol consumption can raise blood pressure and triglyceride levels, a type of fat found in the blood. Alcohol also adds extra calories, which may cause weight gain, especially around the abdomen, which is directly associated with risk of a heart attack (Akil and Ahmad 2011). Cigarette smoking also increases the risk of coronary heart disease. Nicotine increases blood pressure; in addition, cigarette smoke causes fatty buildup in the main artery in the neck and thickens blood, making it more likely to clot. It also decreases levels of HDL (“good”) cholesterol (American Heart Association 2014). Even secondhand smoke can have an adverse effect if exposure occurs on a regular basis. Chronic psychological stress also elevates the risk of heart disease (Dimsdale 2008). The repeated release of stress hormones like adrenaline elevates blood pressure and may eventually damage artery walls. The human and its connections to health and disease are discussed in more detail below.
OSTEOARTHRITIS
The appearance of osteoarthritis in skeletal remains from the Neolithic has been attributed to the repetitive loading of articular joints due to the manual labor associated with early agricultural production (Larsen 2014). In modern populations, overweight and obesity are major contributing factors to arthritis, due not only to the overloading of joints that comes with excess weight (Guilak 2011) but also to the action of fat cells that generate low-level inflammation in response to high levels of glucose in the blood (Issa and Griffin 2012). Meaning, diabetes is a risk factor for osteoarthritis (Berenbaum 2011). A high percentage of obese individuals with knee osteoarthritis are sedentary, suggesting lack of physical activity may increase susceptibility to inflammation (Issa and Griffin 2012). Again, excess body weight and lack of physical activity are a mismatch for Stone Age bodies making their way in the space age (Eaton et al. 1988).
CANCER
Cancer is the second-leading cause of death globally, causing one in every six deaths and killing nearly nine million people in 2015 (WHO 2018b). Lifetime cancer risk in developed Western populations is now one in two, or 50% (Greaves 2015). Approximately one-third of deaths from cancer are due to behavioral and dietary factors, including high Body Mass Index (BMI), low fruit and vegetable intake, lack of physical activity, and the use of tobacco and alcohol. Depending on the type of cancer and one’s own genetic inheritance, these factors can increase cancer risk from 2- to 100-fold (Greaves 2015). Cancer is the result of interactions between a person’s genes and three categories of external agents: physical carcinogens (e.g., ultraviolet radiation), chemical carcinogens (e.g., tobacco smoke, asbestos), and biological carcinogens, such as infections from certain viruses, bacteria, or parasites (WHO 2018b). Obesity is also a risk factor for cancer, including of the breast, endometrium, kidney, colon, esophagus, stomach, pancreas, and gallbladder (National Institutes of Health 2017; Vucenik and Stains 2012).
Cancer has been regarded as a relatively recent affliction for humans that became a problem after we encountered exposure to modern carcinogens and lived long enough to express the disease (David and Zimmerman 2010). Given the long history that humans share with many oncogenic (cancer-causing) parasites and viruses (Ewald 2018), and the recent discovery of cancer in the metatarsal bone of a 1.8-million-year-old hominin (Odes et al. 2016), this view is being challenged (See Special Topics). The difficulties of identifying cancer in archaeological populations are many. Most cancer occurs in soft tissue, which rarely preserves, and fast-growing cancers would likely kill victims before leaving evidence in bone. It is also difficult to distinguish cancer from benign growths and inflammatory disease in ancient fossils, and there is often post-mortem damage to fossil evidence from scavenging and erosion. In light of these challenges, Paul Ewald (2018) suggests using other lines of evidence to discern the prevalence of cancer in ancient humans, including examining the history of cancer-causing parasites and viruses. His complete analysis is beyond the scope of this chapter, but one example of a virus you may be familiar with will serve to illustrate the concept.
SPECIAL TOPIC
Earliest evidence of cancer in hominins: Using 3-D images, South African researchers diagnosed a type of cancer called osteosarcoma in a toe bone belonging to a human relative who died in Swartkrans Cave between 1.6 and 1.8 million years ago. https://news.nationalgeographic.com/2016/07/oldest-human-cancer-disease-origins-tumor-fossil-science/
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States, and 79 million Americans, most in their late teens and early twenties, are infected with HPV (CDC 2017). HPVs are transmitted through sexual activity and can cause cancers of the cervix, vulva, vagina, penis, or anus. It can also cause cancer in the back of the throat, including at the base of the tongue and tonsils. The Centers for Disease Control recommends all 11–12 year olds, both girls and boys, get two doses of the HPV vaccine to protect against diseases, including cancers, caused by HPV. One such disease is cervical cancer, the fourth-leading cause of death for women in the world, and the second most common cause of death by cancer (surpassed only by breast cancer) for women ages 15–44 (Bruni et al. 2017). There are over 100 different strains of HPV, but Types 16 and 18 cause 70% of all cervical cancers (Bruni et al. 2017). Type 16 is the most oncogenic of the HPVs, and it has been present in the genus Homo for half a million years, suggesting cervical cancer and other cancers caused by HPV may have been too (Ewald 2018).
Behavioral or “lifestyle” choices have an impact on cancer risk. Breast cancer is one example. It is the most common cancer in women worldwide, but of new cases varies from 19.3 per 100,000 women in Eastern Africa to 89.7 per 100,000 women in Western Europe (WHO 2018b). These differences are attributable to cultural changes among women in Western, industrialized countries that are a mismatch for our evolved reproductive biology. Age at , the onset of menstrual periods, has dropped over the course of the last century from 16 to 12 years of age in the U.S. and Europe, with some girls getting their periods at nine or ten years old and developing breasts as young as eight years old (Greenspan and Deardorff 2014). A World Health Organization study involving data from 34 countries in Europe and North America suggests the primary reason for the increase in earlier puberty is obesity, with differences in Body Mass Index (BMI) accounting for 40% of individual- and country-level variance (Currie et al. 2012). Exposure to hormone-disrupting chemicals in utero and childhood may also be a factor (Greenspan and Deardorff 2014). As with other aspects of health discussed in this chapter, social and economic factors also influence earlier puberty, with girls who grow up in homes without their biological father twice as likely to experience early puberty, as is the case for girls who experience childhood trauma and/or grow up in a home with a depressed mother (Greenspan and Deardorff 2014). There is also ethnic variation in early puberty, with African American and Latina girls much more likely to experience puberty at younger ages. These factors combine in that African American and Latina girls are more likely to be overweight or obese and to grow up in low-income neighborhoods, where they are more likely to be exposed to environmental pollutants. Early puberty in girls has been associated with increased risk of breast cancer, ovarian cancer, obesity, diabetes, and raised triglycerides in later life (Pierce and Hardy 2012). In addition, there are negative social consequences, with girls who develop early more likely to experience anxiety, depression, poor body image, and eating disorders (Greenspan and Deardorff 2014).
At the same time, age at puberty is dropping for girls in Western nations and age at birth of the first child is later, on average at 26 years old (Mathews and Hamilton 2016). Women are also having fewer children, two on average (Gao 2015), with 15% of women choosing to remain childless (Livingston 2015). Rates of breastfeeding have risen in recent decades but drop to only 27% of infants once babies reach 12 months of age (CDC 2014). Nearly one-third of women also take oral contraceptives or use another hormonal method of birth control (Jones and Dreweke 2011). In contrast, data from modern foraging populations (Eaton et al. 1994) indicate age at menarche is around 16 years old, age at birth of the first child is 19, breastfeeding on-demand continues for three years for each child, and the number of live births to women who survive to age 60 averages six. These differences relate to elevated risk for reproductive cancers among women in developed countries.
Other than an established genetic risk (e.g., BRCA gene), the primary risk factor for breast cancer is exposure to estrogen. For women living in modern, industrialized economies, this exposure now often comes from women’s own ovaries rather than from external environmental sources (Stearns et al. 2008). There is nothing biologically normal about regular monthly periods. Women in cultures without contraception are pregnant or lactating (breastfeeding) for much of their reproductive lives, resulting in 100 or so menstrual cycles per lifetime. In contrast, Western women typically experience 400 or more (Strassmann 1997). This is partly due to younger ages at menarche. From menarche to the birth of a woman’s first child can be 14 years or longer in modern, Western populations, after which breastfeeding, if undertaken at all, lasts for a few weeks or months and is not on-demand, negating the natural birth control provided by frequent lactation. Women may also choose to use oral contraceptives or other hormonal methods to control reproduction. In their current form, these drugs induce a monthly period. Age at menopause (the cessation of menstrual cycles) is constant at 50–55 years old across human populations. For Western women, this translates into forty years of nearly continuous menstrual cycling between menarche and menopause. Each month the body prepares for a pregnancy that never occurs, increasing cell divisions that put women at risk for cancers of the breast, endometrium, ovaries, and uterus (Strassmann 1999). Obesity adds to this risk, as obese women have greater proportions of bioavailable estrogen (Eaton et al. 1994). In obese and overweight postmenopausal women, adipose (fat) tissues are the main source of estrogen biosynthesis. Thus, weight gain during the postmenopausal stage means higher exposure to estrogen and greater risk of cancer (Ali 2014). Factors associated with reduced risk of reproductive cancers are late menarche, early first birth, high numbers of pregnancies, early menopause, and breastfeeding.
Again, humans cannot return to our evolutionary past, and there are important social and economic reasons for delaying pregnancy and having fewer children. These include achieving educational and career goals, leading to greater earning power and a reduction in the gender pay gap, as well as more enduring marriages and a decrease in the number of women needing public assistance (Sonfield et al. 2013). There are also cultural means by which we might reduce the risk of reproductive cancers that do not involve increases in family size. These include reformulating hormonal contraceptives with enough estrogen to maintain bone density and stave off osteoporosis, but reducing the number of menstrual periods over the reproductive lifespan (Stearns et al. 2008). Reducing fat intake may also lower serum estrogen concentrations, while high-fat diets have been shown to contribute to breast tumor development. High-fiber diets are also beneficial in decreasing intestinal resorption of estrogenic hormones. Exercise also appears protective, with studies of former college athletes demonstrating risks of breast, uterine, and ovarian cancers later in life two to five times lower than those of non-athletes (Eaton et al. 1994).
SPECIAL TOPIC: THE PALEO DIET
Given the impact of diet on every health condition discussed so far in this chapter, you may be considering changing what you eat. But what diet to follow? Given your interest in human evolution, have you ever wondered about the Paleo diet? Popularized by the 2002 book, The Paleo Diet: Lose Weight and Get Healthy by Eating the Food You Were Designed to Eat, by professor of nutrition and exercise physiology Loren Cordain, the Paleo diet is an eating plan based on the idea that eating like our ancestors is protective against weight gain, metabolic disorders, and other maladies of modern life. Its publication spawned an entire industry of diets, exercise plans, cookbooks, and other products based on the “Paleolithic prescription.”
Recommendations of the Paleo diet include eating high amounts of protein, fewer carbohydrates, more fiber, certain fats, and foods rich in plant phytochemicals, vitamins, minerals, and antioxidants. Sounds good so far, but let’s dive a little deeper. Protein in the Paleo diet consists of lean meats (including organ meats), fish, and seafood. And not industrially produced versions of these. The meat should be grass- not grain-fed, and the fish should be wild caught, not farmed. All fruits are included in the diet, but only non-starchy vegetables make the cut, meaning no tubers like potatoes. The recommended carbohydrates have a low Glycemic Index, meaning they are more slowly digested and metabolised causing a lower, slower rise in blood glucose and insulin levels. There are also no cereals, no legumes (beans), no dairy products, no processed foods, no refined sugars (including honey), and no added salt. The primary fats in the diet are monounsaturated, polyunsaturated, and omega-3 fats, rather than the trans fats and saturated fats most often found in contemporary diets (Cordain 2002).
Particular attention is given to counteracting what many people think of as high-protein foods. Hamburger, eggs, and cheese, which are 24%, 34%, and 28% protein, respectively, are off the list, as opposed to skinless turkey breast (94% protein) and shrimp (90%). There is also the idea that current Western diets are more acidic than alkaline, reducing calcium levels in the body by promoting excretion of calcium in the urine. Cereals, dairy products, legumes, meat, fish, eggs, and salty processed foods elevate acid loads in the body, while fruits and non-starchy vegetables produce net alkaline loads. The diet advises eating 35% of your daily calories as fruits and veggies to balance out the high recommended protein intake. These recommendations are based on the premise that this represents a typical diet of hunter-gatherers in our ancient past before the transition to agriculture. Given what you have learned about human evolution from this text, what might be some problems with this assumption? How about with the diet itself?
To begin, there is no such thing as the Paleo diet. Hominins occupied a variety of ecological niches, with corresponding variety in what they ate (Lucock et al. 2014), including wide variation in their consumption of meat (Wrangham 2009). There is also archaeological evidence and dietary analysis of teeth demonstrating that hominin foragers ate cooked grains as far back as two million years ago (Zuk 2013). Although modern foragers are not an analogue for the past, they vary widely in their dietary intake. Meat forms 99% of the traditional Inuit diet (McElroy and Townsend 2009), while the diet of the !Kung of sub-Saharan Africa is mostly vegetarian (Lee 2013). In the case of the Inuit, they have genetic mutations related to the processing of omega-3 fatty acids that allow them to live on such a high-protein, high-fat diet without the cardiovascular disease and metabolic issues found in other populations (Fumagalli et al. 2015). Similarly, some pastoral populations became lactase persistent over time, allowing their members to digest milk as adults (Crow and Kimura 1970), and there are genotypes favored among peoples with high-starch diets that improve the digestion of starches (Marciniak and Perry 2017) and promote resistance to infectious disease (Lucock et al. 2014). Clearly, not all humans ate the same things, and natural selection favored genotypes that allowed populations to survive as they encountered new food sources and their diets changed. The modern Paleo diet also does not take into account the difficulty of procuring the lean protein that it recommends in the absence of hunting it yourself. Furthermore, it leaves out fermented foods, like pickled vegetables, yogurt, and cheeses, that contribute to a healthy microbiome (Graber 2014), something researchers are coming to find is essential to health (Shreiner et al. 2015).
What, then, to eat? As with Paleo diets, what humans eat today varies by geography, economics, and cultural preferences, among other factors. The burgeoning science of nutrigenomics hopes to one day be able to provide each individual with a customized diet based on analysis of your own DNA, lifestyle, and disease risk (Neeha and Kinth 2013). Until that time, World Health Organization dietary recommendations for the prevention of chronic diseases like cardiovascular disease, diabetes, and cancer emphasize diets that are low in saturated fat, salt, and sugar, high in fiber, and feature lean proteins (including nuts and fish) and carbohydrates from whole grains, legumes (beans), fresh fruits, and vegetables (WHO 2018c). Fiber, in particular, has been shown to be protective. Epidemiological and clinical studies demonstrate that intake of dietary fiber from plants and whole grains is inversely related to obesity, Type 2 diabetes, colon cancer, and cardiovascular disease (Lattimer and Haub 2010). Newer research suggests diets high in fiber also boost immune function, mood, and cognition (Kaczmarczyk et al. 2012).
Can these recommendations be met with a vegetarian or vegan diet? Research suggests this is the case, if one is conscientious and knowledgeable about the combination and timing of foods to obtain essential nutrients (McEvoy et al. 2012; Woo et al. 2014). Research introduced earlier in this chapter regarding the negative health effects of cooked meats suggests that eating meat four times per month or less, eating it rare, and avoiding processed meats altogether, is less likely to result in cancer, diabetes, and hypertension (Abid et al. 2014; Liu 2018; Liu et al. 2018; Trafialek and Kolanowski 2014). Additionally, according to the EAT-Lancet Commission on healthy diets from sustainable food systems, global consumption of foods such as red meat and sugar will have to decrease by half to make sure the Earth will be able to feed a growing population of 10 billion people by 2050. At the same time, people will need to double the amount of plant-based foods they eat, including nuts, fruits, vegetables, and legumes (Willett et al. 2019).
STRESS
Have you ever been “stressed out” in class? Say you’re in a large lecture hall with a hundred other people, or even in a small class where you don’t know anyone. You’re not sure about something the professor just said and you would really like to ask about it, so you start to raise your hand. Does your heart begin to pound and your mouth get dry? Do you sometimes get so nervous you choose to catch up with a classmate after lecture instead? If so, you are not alone. Fear of speaking in public is one of the most common social phobias (APA 2013). It has been estimated that 75% of all people experience some degree of anxiety or nervousness when it comes to public speaking (Hamilton 2011), and surveys have shown that most people fear public speaking more than they fear death (Croston 2012).
We have evolution to thank for this.
Humans, like other primates, are social animals. Being part of a group helped us to survive predation, get enough to eat, and successfully raise our young. When faced with standing up in front of a group, or even speaking up in class, we break into a sweat because we are afraid of rejection. Psychologist Glenn Croston (2012) writes, “The fear is so great because we are not merely afraid of being embarrassed or judged. We are afraid of being rejected from the social group, ostracized and left to defend ourselves all on our own. We fear ostracism still so much today it seems, fearing it more than death, because not so long ago getting kicked out of the group probably really was a death sentence.” Hence, it is no surprise that public speaking triggers a stress response among much of humankind.
The human nervous system evolved in a context where quick responses to perceived threats presented an evolutionary advantage. The “fight or flight” response with which we are all familiar was honed during millions of years when threats more often took the form of an approaching lion than an approaching deadline. Our body’s response, however, is triggered by a wide variety of stressors that produce the same general pattern of hormonal and physiological adjustments (Martini et al. 2013). In today’s world, the system is often stuck in the “on” position due to the constant pressures of modern life, and this is a significant influence on health and disease.
The human stress response involves the acting in concert with the and . It includes three phases: alarm, resistance, and exhaustion (Martini et al. 2013). The alarm phase is the automatic, short-term response to a crisis, the “fight or flight” response you might have experienced when thinking about raising your hand in class. Epinephrine is the dominant hormone of this phase. Its secretion stimulates activation of the sympathetic nervous system, including sudden increases in heart rate, respiration, mental alertness, sweat gland excretion, and energy use. If the stress-inducing situation lasts more than a few hours, the body shifts to the resistance phase. Glucocorticoids are the dominant hormones of this phase, which involves mobilizing the body’s metabolic reserves to maintain the energy levels necessary for the brain to function during continued stress. A side effect of glucocorticoids is suppression of inflammation and the immune response, and cardiovascular damage can occur from elevations in blood pressure and blood volume from the action of ADH (antidiuretic hormone) and aldosterone (a hormone that regulates salt and water in the body). The resistance phase can be maintained for weeks or months, but eventually homeostatic regulation breaks down and leads to the exhaustion phase. If corrective actions are not taken, organs begin to fail, and death follows (Martini et al. 2013).
The negative effects of sustained, elevated cortisol levels on health are well documented. These include higher levels of infectious disease and slowed growth in childhood (Flinn and England 2003) and increased incidence of heart disease, obesity, and diabetes in adults (Worthman and Kuzara 2005). As opposed to what might have been the case in our evolutionary past, many causes of sustained stress in contemporary societies are psychosocial rather than physical threats. These can include an unhappy marriage or frustrations at work (Dimsdale 2008). Stressors can also be more subtle. For example, a recent review of research into the effects of stress on health indicated internalized racism was a significant stressor that was positively associated with alcohol consumption, psychological distress, overweight, abdominal obesity, and higher fasting-glucose levels among minority groups (Williams and Mohammed 2013). Chronic everyday discrimination is also positively associated with coronary artery calcification, elevated blood pressure, giving birth to lower-birth-weight infants, cognitive impairment, poor sleep, visceral fat, and mortality. These effects have been shown to increase morbidity and mortality among members of affected groups.
Epigenetics can also be a factor in how a person is able to deal with stressful situations. Maternal experiences of stress during pregnancy have the potential to permanently alter the physiology of mothers’ offspring, especially the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis regulates metabolism, blood pressure, and the immune response, and these alterations can predispose prenatally stressed individuals to suffer metabolic, cardiovascular, and mental disorders in adulthood (Palma-Gudiel et al. 2015). These experiences carry across generations, with children of Holocaust survivors who experienced PTSD demonstrating similar changes in neurochemistry in the absence of a sustained, traumatic event, as did infant offspring of mothers who developed PTSD during pregnancy after witnessing the traumatic events of 9/11 (Yehuda and LeDoux 2007). Clearly, stress has a profound impact on human health and is one more example of a biological system that is maladaptive in many modern contexts.
SYNDEMICS AND THE ECOLOGICAL MODEL
It is important to recognize that disease risk is not spread evenly within or between populations. Diseases also combine and interact to create a , where the coexistence of two or more conditions exacerbates the effects of one or all conditions. One example is coinfection with HIV and Mycobacterium tuberculosis, which is associated with more rapid disease progression, worse symptoms, and a higher pathogenic load than during a single infection with either agent (Singer et al. 2017). Syndemic risk also includes social, political, economic, and environmental factors that increase risk for the clustering of two or more diseases (Singer et al. 2017; Singer and Clair 2003). One of the first syndemics identified involved substance abuse, violence, and AIDS (SAVA), in which the inner-city health crisis around HIV/AIDS was related to other conditions, including tuberculosis, sexually transmitted infections, hepatitis, cirrhosis, infant mortality, drug abuse, suicide, and homicide. These were, in turn, connected to poverty, homelessness, unemployment, poor nutrition, lack of social support, and social and ethnic inequality (Singer et al. 2017). Together, these factors and others, like health policy and unequal access to health care, form an of health and disease, a more holistic way of viewing health issues and their solutions than focusing solely on biology and medical intervention (Sallis et al. 2008).
A historical example will serve to illustrate these concepts. You will remember the discussion of the first epidemiological transition from earlier in this chapter. This involved a rise in infectious disease following human adoption of agriculture as a primary subsistence strategy. This transition took place in the Old World and was fueled by zoonotic pathogens that infected humankind following the domestication of cattle, pigs, horses, sheep, goats, chickens, and other species. During the thousands of years following that transition, epidemics repeatedly occurred among Old World populations resulting in periods of crisis mortality, when large numbers of people died. This was followed by population recovery as survivors, who often became immune to reinfection, produced new generations to be infected during the next epidemic (Omran 2005). This same set of interactions did not, however, occur in the New World, where species that might have developed into domesticated animals equivalent to horses and cattle were wiped out at the end of the last Ice Age, when humans are hypothesized to have migrated to the New World across an exposed land bridge in the Arctic (Diamond 1997). These extinctions may have been the result of hunting or climate change or a combination of both. What is important to note is that the land bridge disappeared as sea levels rose at the end of the Ice Age, isolating the Americas until European contact in the 15th century. This isolation was to have severe consequences for Native Americans.
When Columbus “discovered” the New World in 1492, he unleashed one of the first waves of infectious disease that decimated Native American populations in the centuries to follow (Crosby 2003), eventually killing 90% of the population, an estimated 20 million people (Diamond 1997). The devastation of native communities was the result of a combination of factors. One was the very different histories of Europe and the Americas. With no history of animal domestication beyond dogs, turkeys, ducks, guinea pigs, llamas, and alpacas, Native Americans did not fall prey to zoonotic pathogens that produced highly contagious infectious diseases, leaving them with no resistance. Also, in spite of their profound differences in culture, language, subsistence, and political and economic systems, Native Americans were genetically very much alike (Crosby 2003). This was due to the small number of individuals who crossed the land bridge, which then closed, leaving them in genetic isolation for 10,000 years or more. This meant there was not a high degree of variation for natural selection to act upon in the midst of the severe evolutionary pressure of smallpox and other infectious diseases introduced by Europeans. Native Americans had also not benefited from the technological developments associated with warfare in the Old World, including steel swords, guns, and fighting on horseback, that had been perfected over centuries of conflict (Diamond 1997). European conquest also toppled existing political and social systems already crippled by epidemics of disease, leading to social disorder and cultural and economic disruption. To compound the situation, European colonization included the enslavement and forced labor of native populations to serve European interests, resulting in injury, starvation, and other mistreatment and leading to further loss of life. This complex of epidemiological, technological, social, political, and economic factors (a syndemic) combined to nearly exterminate Native Americans in the centuries following European contact, but this need not have been the case. Alfred Crosby (2003) points out that although epidemics among immunologically unprepared populations produce high mortality rates, some individuals survive, and the population will recover if left alone. He reminds us that,
Europe, for instance, lost one-third of its population to the Black Death in
the fourteenth century and recovered in time. If the Black Death had been
accompanied by the arrival of Genghis Khan’s hordes, miraculously plague-proof,
the story would have been very different. It might have been similar to what
happened when European settlers followed on the heels of smallpox and other
infections previously unknown to American Indians. [Crosby 2003:xxii]
Unfortunately, syndemics did not begin or end with European colonization of the New World. Interactions between disease and income inequality, education, discrimination, warfare, migration, climate change, and a host of other factors continue to affect humans today, causing health disparities that lead to differences in morbidity and mortality within and across nations (Singer and Baer 2012; see Figure 16.9).
|
United States |
Worldwide |
|
1. Heart disease |
1. Heart disease |
|
2. Cancer |
2. Stroke |
|
3. Accidents |
3. Chronic Obstructive Pulmonary Disease |
|
4. Chronic lower respiratory diseases |
4. Lower respiratory infections |
|
5. Stroke |
5. Alzheimer disease and dementia |
|
6. Alzheimer’s disease |
6. Lung cancer |
|
7. Diabetes |
7. Diabetes mellitus |
|
8. Influenza and pneumonia |
8. Road injury |
|
9. Kidney disease |
9. Diarrheal diseases |
|
10. Suicide |
10. Tuberculosis |
Figure 16.9 Top ten causes of death in the U.S. and worldwide.
Although a full discussion of global health disparities is beyond the scope of this chapter, a brief discussion of asthma in the United States can shed light on several common factors that contribute to inequalities in health today. Nearly 20 million people in the U.S. suffer from asthma, over a third of whom are children under 18 years of age (CDC 2017). Childhood-asthma prevalence doubled from 1980 to 1995, then increased slowly from 2001 to 2010, leveling off in 2013. Rates of asthma are highest among African American and Latino children (Akinbami et al. 2016). Among Latinos, Puerto Ricans have the highest lifetime asthma rate (16.9%), more than three times the rate for Mexican Americans (Singer and Baer 2012). Given that most adult asthma has its origins in early life, discovering the causes of childhood asthma and preventing it has become a major public health focus (Beasley et al. 2015).
A range of factors contribute to the development of asthma in childhood. These include genetics and family history, as well as exposure to stress and being born into a single-parent family. Other factors include being a low-birth-weight baby or being born prematurely. Living in an urban environment, being exposed to indoor and outdoor air pollution, including cigarette smoke, is also a contributor. Certain childhood infections (e.g., pertussis), antibiotics use, and exposure to environmental toxins like mold are also associated with asthma. Diets high in trans-fatty acids and salt, especially fast-food, also contribute to the development of asthma. Sedentarism, high BMI, overweight, and obesity are also factors, with incidence increased by 20% in overweight children and doubled for obese kids (Chen et al. 2012). There are also gender differences associated with the obesity-asthma connection, with boys experiencing higher rates until age 13 and asthma becoming more prevalent in girls post-puberty (Beasley et al. 2015). The mechanisms behind this are unknown but may include anatomical differences in lung capacity, sleep disorders, body fat distribution, and inflammation (Chen et al. 2012). In keeping with the hygiene hypothesis, children exposed to dogs or farm animals in early childhood, including before age one, are less likely to develop asthma (Fall et al. 2015), especially children in urban environments where they may have less frequent contact with the natural environment (Dunn 2018).
Differences in prevalence of childhood asthma between ethnic groups within a population are not mainly because of genetic differences but, rather, because of differences in exposure to environmental and lifestyle factors (Beasley et al. 2015). Given this, let us examine the case of African American and Latino children in light of the risk factors just described. Working-class people and people of color in the U.S. are more likely to live in close proximity to freeways and environmental threats like petrochemical plants and waste incinerators. They are also more likely to live in poverty and in areas with high rates of crime and violence, which elevate stress levels, as does racial discrimination (Singer and Baer 2012). African American children are also far more likely than other groups in the U.S. to grow up in female-headed households, with 72% now being born to single mothers (Washington 2010), many of whom live in poverty and lack access to health care (Pearl 2015). Accurate diagnosis and treatment are key to management of childhood asthma, yet many children of color remain undiagnosed, in part because of lack of regular check-ups. One study conducted among Puerto Ricans in Chicago found prevalence of asthma among Puerto Rican children jumped to 34% when counting cases of possible asthma based on reports of patient symptoms rather than a physician’s diagnosis (Joseph et al. 1996). Another study, conducted in New York City, demonstrated that Puerto Rican children were more likely to miss school because of asthma than other ethnic groups in the same neighborhoods, and that low-income Latino families with children with asthma were less likely to have training, education, and resources to manage their child’s asthma (Findley et al. 2003). A 2002 study of over 1,000 American children and their families found that Latino and African American children were less likely to be prescribed the standard treatment for asthma and that Latino children received fewer inhaled steroids than white children (Ortega et al. 2002). Clearly, there are multiple factors contributing to health disparities in asthma for American children of different ethnic backgrounds, suggesting an ecological approach is necessary for addressing the problem.
Currently, there is no cure for asthma and no vaccine against it. Instead, public health efforts have largely focused on diagnosis, treatment, and education in place of prevention (Beasley et al. 2015). Given the sheer number of risk factors involved, some scholars have begun to question whether prevention is even possible. Richard Beasley and colleagues (2015:1078) explain: “Public health efforts will need to focus on reducing environmental tobacco exposure, reducing indoor and outdoor air pollution and occupational exposures, reducing childhood obesity and encouraging a diet high in vegetables and fruit, improving fetal and maternal health, encouraging breastfeeding, promoting childhood vaccinations, and reducing social inequalities.” These challenges serve to remind us to take an ecological approach to health and disease. As humans, we all have our biology and genetics with which to contend, but we often do so in the midst of very different life circumstances.
ARE WE STILL EVOLVING?
Given the current global burden of non-communicable diseases like heart disease, cancer, and diabetes discussed in this chapter, many students ask why humans have not yet evolved in response. First, the health conditions highlighted here do not typically have repercussions on reproductive success, meaning natural selection cannot act to favor one genotype over another to protect against them. There also may not have been sufficient time for natural selection to act (Stearns et al. 2008). The cultural transformation of our food supply and lifestyle came about quickly. The transition from foraging to farming took place beginning 12,000 years ago, industrial food production came about in the last 200 years, and technologies like television, the internet, and social media that promote sedentarism are less than 75 years old—one human lifetime. Even under the strongest selective pressure, evolution takes many generations. For example, the mutation that led pastoral populations to be able to digest fresh milk likely took 8,000 years, or 325 generations, to reach a frequency of 90% (Crow and Kimura 1970). This does not mean, however, that humans have stopped evolving. As a species, we continue to respond to selective pressures biologically and culturally. This portion of the chapter will focus on contemporary examples of human evolution.
Before beginning, let’s remind ourselves of the modern definition of evolution, which is a change in allele frequencies across generations in a given population for a particular trait. We must also review the conditions necessary for natural selection to operate on a trait. First, the trait must be heritable, meaning it is transmitted genetically from generation to generation. Non-inherited traits are learned and include things like cultural preferences for certain types of foods or who we think it is best to marry. Not only must a trait be heritable, there must also be variation of the trait in human populations and the trait must influence reproductive success. Three examples of traits that meet these criteria are immunity to HIV, height, and wisdom teeth (Andrews et al. 2011).
AIDS is a potentially fatal infectious disease caused by the Human Immunodeficiency Virus (HIV), a zoonosis believed to be derived from Simian Immunodeficiency Viruses (SIVs) found in chimpanzees and monkeys, most likely transmitted to humans through the butchering of infected animals (Sharp and Hahn 2011). In total, 35 million people have died from AIDS-related illnesses since the start of the global epidemic in the 1980s. There were 36.7 million people around the world living with AIDS as of 2016, including 1.8 million new cases and 1 million deaths in that year alone (UNAIDS 2018). A disease causing this level of morbidity and mortality represents a major selective pressure, especially given that infection can occur before birth (Goulder et al. 2016), having an affect on future reproductive success.
The majority of people in the world are highly susceptible to HIV infection, but some are not. There are individuals who are homozygous for a rare, recessive allele at the CCR5 locus who are immune. Heterozygotes who inherit a single copy of this allele are more resistant to infection and the disease takes longer to progress in the event they are infected. The mechanism by which the allele prevents infection involves a 32-base pair deletion in the DNA sequence of the CCR5 gene, creating a non-functioning receptor on the surface of the cell that prevents HIV from infecting the cell. The allele is inherited as a simple Mendelian trait, and there is variation in its prevalence, ranging as high as 14% of the population in northern Europe and Russia (Novembre et al. 2005; see Figure 16.8). What is interesting about the allele’s geographic distribution is that it does not map onto parts of the world with the highest rates of HIV infection (UNAIDS 2018), suggesting that AIDS was not the original selective pressure favoring this allele (Figure 16.10 and Figure 16.11).


Given its current geographic distribution, the bubonic plague, which ravaged Europe repeatedly from the 14th to the 19th centuries (Pamuk 2007), was initially proposed as the selective agent. Subsequent research suggests smallpox, which killed up to 400,000 people annually in 18th-century Europe (Hays 2005), was more likely the selective pressure (Novembre et al. 2005). Given the mortality rates for smallpox and the selective pressure it has exhibited on humanity for centuries (Crosby 2003), an allele that conferred immunity was highly advantageous, as it is for those faced with the threat of HIV infection today. There are efforts to employ the natural immunity this mutation provides in the creation of an AIDS vaccine (Lopalco 2010).
Height is another example of a trait currently experiencing selective pressure. If you have ever toured a historical site, you have likely hit your head on a doorframe or become claustrophobic trying to squeeze down a narrow hallway under a lower-than-average ceiling. It is not your imagination. Humans have gotten taller in recent centuries. In fact, the average height of people in industrialized nations has increased approximately 10 centimeters (about four inches) in the past 150 years. This increase has been attributed to improvements in nutrition, sanitation, and access to medical care (Hatton 2014). But this is only part of the story.
Height is highly heritable. Studies indicate 80% of variation in height within populations is due to genetics, with 697 different genetic variances identified as having an effect on adult stature (Devuyst 2014). Multiple studies also demonstrate a positive relationship between height and reproductive success for men (Andrews et al. 2011). This is primarily due to sexual selection and nonrandom mating, namely women’s preferences for taller men, which may explain why height is one characteristic men often lie about on dating websites (Guadagno et al. 2012). Sexual selection also plays out with regard to economic success in Western cultures, with taller men more likely to be in higher-level positions that pay well. Research demonstrates an inch of height is worth an additional $789 per year in salary, meaning a man who is six feet tall will earn on average $5,525 more per year than an identical man who is five foot five (Gladwell 2007). Over the course of a thirty-year career, this adds up to hundreds of thousands of dollars, likely allowing the taller man to attract more potential mates and increase his reproductive success.
Wisdom teeth are also undergoing evolutionary pressure. Have you or anyone in your family had their wisdom teeth removed? It can be a painful and expensive process, and it is a common experience in Western nations. Conversely, do you know anyone whose wisdom teeth never came in? That is fairly common in other populations, suggesting evolutionary pressure favoring the absence of wisdom teeth has been culturally influenced. According to research by physical anthropologists, the oldest fossil evidence of skulls missing third molars was found in China and is 300,000 to 400,000 years old, suggesting the earliest mutation selecting against the eruption of wisdom teeth arose in Asia (Main 2013). Since that time, jaws have continued to decrease in size to the point they often cannot accommodate third molars, which can become impacted, painful, and even infected, a condition physical anthropologist Alan Main argues might have interfered with the ability to survive and reproduce in ancestral populations (Main 2013). As we have learned, a mutation that positively influences reproductive success—such as being born without the trait to develop wisdom teeth in an environment where food was cooked before eating—would likely be selected for over time. Evidence in modern humans suggests this is the case, with 40% of modern Asians and 45% of Native Alaskans and Greenlanders (populations descended from Asian populations) lacking wisdom teeth. The percentage among those of European descent ranges from 10 to 25% and for African Americans is 11% (Main 2013). Earlier chapters in this text emphasize that directional selection progresses along a particular path until the environment changes and a trait is no longer advantageous. In the case of wisdom teeth, the ability of modern dentistry to preempt impaction through surgery may, in fact, be what is preventing natural selection from doing away with wisdom teeth altogether.
FOOD FOR THOUGHT
This chapter focused on health conditions prevalent in contemporary, industrialized societies that are due, in part, to the mismatch between our evolved biology and modern cultural and physical environments. Obesity is at the root of it all. Claude Bouchard (2007) identified factors contributing to the global epidemic of obesity and the diseases associated with it. These are the built environment and the social environment, which together form the obesogenic environment in which unhealthy behaviors are encouraged. This chapter will close by examining each of these in a college context.

In terms of the built environment, consider your campus or neighborhood from an evolutionary perspective. To what degree does the construction of the space lend itself to physical activity as part of daily life? Is your campus constructed in such a way that it promotes the use of automobiles at the expense of walking or biking? If driving is necessary, is parking available close to the buildings or do you need to walk a fair distance from the parking lot to your destination? Do the buildings have stairs or ramps or is it necessary to take the elevator? Is it possible to negotiate safely around campus or the neighborhood on foot or by bike in all weather? After dark? How about the classrooms and computer labs? Do they have standing or treadmill desks as options? Does your class schedule encourage walking from building to building between classes, or are most courses in your major scheduled in the same location? I regularly have students who sit in the same room for hours, not even changing desks, while instructors rush from place to place. Most college majors also lack a physical activity requirement, leaving it up to students to incorporate exercise into already-busy schedules (See Figure 16.12).
Sociocultural factors that contribute to obesity include food advertising, ubiquitous fast-food and junk food options, and social pressure to consume, all of which are present on college campuses. Although nutritional options on campuses have improved in recent years, many students find eating healthy in the dining halls and dorms challenging (Plotnikoff et al. 2015), and students who live off campus fare even worse (Small et al. 2013). There are also parties and other social events, a normal part of college life, that often involve unhealthy food and encourage behaviors like alcohol consumption and smoking. Give some thought to the social atmosphere on your campus and the ways in which it may contribute to obesity. My own freshman orientation involved a succession of pizza parties, ice cream socials, and barbecues, followed by late-night runs to the nearest fast-food outlet. The purpose of these events was to encourage people to make friends and feel comfortable living away from home, but the foods served were not healthy, and there was social pressure to join in and be part of the group. Such activities set students up for the “freshman fifteen” and then some. They also reinforce the idea that being social involves eating (and sometimes drinking and/or smoking).
Sedentarism and inactivity are also built into the academics of college life. Digital technology is a significant contributor to obesity. Students use laptops and cell phones to take notes, complete their work outside of class, and access social media. There are also video games, virtual reality headsets, and streaming television and movies for entertainment. The built environment of college already necessitates that students sit in class for hours each day, then sit at computers to complete work outside of class. The social environment enabled by digital technology encourages sitting around for entertainment. It is telling that we call it “binge watching” when we spend hours watching our favorite shows. Doing so often involves eating, as well as multiple exposures to food advertising embedded in the shows themselves. In these many ways, college contributes to the development of obesogenic behaviors that can have negative health ramifications long after college is over (Small et al. 2013).
In the U.S., the greatest increase in obesity is among young adults aged 18–29 years, a significant percentage of whom are college students (Plotnikoff et al. 2015). Analyses of college students’ behavior across semesters shows consumption of fruits and vegetables drops over time, as does the amount of physical activity, while consumption of sugar-sweetened beverages and fast-food goes up, leading to weight gain at nearly six times the rate of the general public (Small et al. 2013). Realizing this, many colleges and universities have instituted programs to encourage healthier eating and more physical activity among students (Plotnikoff et al. 2015). Some schools have even done away with collegiate sports, which often serve a small percentage of students, in favor of campus-wide efforts at getting everyone active (Tierney 2013). Investigate the options on your campus and take advantage of opportunities. We cannot change our biology, but we can certainly change our habits.
Review Questions
- Geographer, historian, and author Jared Diamond (1987) once referred to agriculture as “the worst mistake in the history of the human race.” Given what you have learned about the health consequences of the domestication of plants and animals for humans, how would you respond to his statement?
- Why do humans like foods that are “bad” for them? Describe the evolutionary underpinnings of our tastes for sugar, salt, and fat.
- How might understanding contemporary disease from an evolutionary perspective benefit medical practitioners in treating their patients?
- Given the size of the world population today, humanity could not return to foraging for subsistence. What can we do to promote healthier food consumption on a world scale? How might we build changes into our physical environments to counter the health risks associated with modern diet and activity patterns?
- Several risk factors for conditions like heart disease, diabetes, and cancer are referred to as “lifestyle factors,” implying these are behavioral choices people make that put them at risk. These include unhealthy eating, lack of physical activity, smoking, and alcohol consumption. To what degree is unhealthy behavior structured by environment? For example, how does being a college student influence your eating habits, physical activity patterns, smoking, and consumption of alcohol?
- Who benefits from the global obesity epidemic? Think about the following industries and institutions: How might the medical establishment profit from obesity? The fitness industry? The diet industry? Fashion? Pharmaceutical companies? Food manufacturers? Advertisers?
- Can you think of any human traits in addition to height, wisdom teeth, and immunity from HIV that might be undergoing selection? How would you go about investigating those traits to find out if this is true?
Key Terms
Autotrophic: Autotrophic organisms are capable of producing their own food using inorganic substances such as light, water, carbon dioxide or chemical energy.
Body Mass Index (BMI): A person’s weight in kilograms divided by the square of their height in meters. The most widely used measure for identifying obesity. The formula using kilograms and meters (or centimeters) is: weight (kg) / [height (m)]2 . The formula using pounds and inches is: 703 x weight (lbs) / [height (in)]2 .
Cancer: A collection of related diseases in which some of the body’s cells begin to divide without stopping and spread into surrounding tissues.
Cardiovascular Disease (CVD): A disease of the heart and blood vessels, often related to atherosclerosis, CVD is a condition in which a substance called plaque builds up in the walls of the arteries, blood vessels that carry blood away from the heart, compromising the flow of blood to the heart or brain.
Central Nervous System: The complex of nerve tissues stemming from the brain and spinal cord that controls the activities of the body.
Circulatory system: The biological system that circulates blood around the body via the heart, arteries, and veins, delivering oxygen and nutrients to organs and cells and carrying waste products away.
Diabetes Mellitus: An endocrine disorder in which high glucose (blood sugar) levels occur over a prolonged period of time. Blood glucose is your body’s main source of energy and comes from the food you eat. Insulin, a hormone made by the pancreas, helps glucose from food get into your cells to be used for energy. Sometimes your body does not make enough—or any—insulin (Type 1 diabetes) or does not take up insulin well (Type 2 diabetes). Glucose then stays in your blood and does not reach your cells.
“Double Burden”: Refers to parts of the world in which there is a prevalence of chronic disease (e.g.,. cancer, heart disease) while, at the same time, there are also high rates of infectious disease due to poverty, malnutrition, poor sanitation, and lack of access to health care, often accompanied by high rates of maternal and child mortality.
Ecological model: Ecological models of health and disease emphasize environmental and policy contexts of behavior, while incorporating social and psychological influences, rather than focusing on individual behaviors. These models encompass multiple levels of influence and can lend themselves to more comprehensive health interventions.
Emerging Infectious Diseases (EIDs): Infections that have recently appeared within a population or those whose incidence or geographic range is rapidly increasing or threatens to increase in the near future. Examples include Ebola, Zika, SARS, and avian (bird) flu.
Endocrine system: Those organs in the body whose primary function is the production of hormones.
Epidemiological transition: A transformation in patterns of disease (morbidity) and death (mortality) among a population.
Glucose metabolism: The body’s evolved mechanism by which we turn food into energy for bodily functions.
Glycemic Index (GI): A system that ranks foods on a scale from 1 to 100 based on their effect on blood-sugar levels. Carbohydrates with a low GI value (55 or less) are more slowly digested and metabolised causing a lower, slower rise in blood glucose and insulin levels.
Hypertension: High blood pressure. Blood pressure is the force exerted by the blood against the walls of the blood vessels. In a blood pressure reading, the top number (usually higher) refers to the systolic pressure, the amount of pressure in your arteries during the contraction of your heart muscle when your heart beats. The bottom number is the diastolic pressure when your heart muscle is resting between beats. Hypertension can lead to severe health complications and increases the risk of heart attack and stroke.
Incidence: The rate at which new cases of a disease occur in a population over a given period of time.
Insulin: A hormone produced in the pancreas that regulates the amount of glucose in the blood. Lack of insulin or the inability to absorb insulin causes diabetes.
Metabolic Syndrome: A cluster of conditions, including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels that occur together, increasing the risk of heart disease, stroke, and diabetes. Lifestyle changes like losing weight, regularly exercising, and making dietary changes can help prevent or reverse metabolic syndrome.
Menarche: The first occurrence of menstruation.
Morbidity: The number of cases of disease per unit of population occurring over a unit of time.
Mortality: The number of deaths attributable to a particular cause per unit of population over a unit of time.
Noncommunicable Diseases (NCDs): Also known as chronic diseases, NCDs tend to be of long duration and are the result of a combination of genetic, physiological, environmental, and behavior factors. The main types of NCDs are cardiovascular diseases (like heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma), and diabetes.
Obesity: A medical condition in which excess body fat has accumulated to the point that it has adverse effects on health. The most widely used measure for identifying obesity is the Body Mass Index (BMI), a person’s weight in kilograms divided by the square of their height in meters. A measure of 30 kg/m2 is considered obese and 25—29 kg/m2 overweight. Distribution of body fat also matters. Fat in the abdominal region has a stronger association with Type 2 diabetes and cardiovascular disease, meaning waist to hip ratio and waist circumference are also important indicators of obesity-related health risk.
Obesogenic: Promoting excessive weight gain. For example, an environment in which tasty, cheap food filled with excess calories is abundant.
Omnivorous: Able to eat and digest foods of both plant and animal origins.
Osteoarthritis: Refers to the degeneration of joint cartilage and underlying bone, causing pain and stiffness. In the absence of previous injury, it is most common in modern populations from middle age onward.
Prevalence: The proportion of individuals in a population who have a particular disease or condition at a given point in time.
Sedentism: Living in groups settled permanently in one place.
Sedentarism: A way of life characterized by much sitting and little physical activity.
Stress response: A predictable response to any significant threat to homeostasis. The human stress response involves the central nervous system and the endocrine system acting together. Sudden and severe stress incites the “flight or flight” response from the autonomic nervous system in conjunction with hormones secreted by the adrenal and pituitary glands, increasing our heart rate and breathing and releasing glucose from the liver for quick energy.
Stroke: A stroke occurs when a blood vessel leading to the brain is blocked or bursts, preventing that part of the brain from receiving blood and oxygen, leading to the death of cells in that part of the brain.
Syndemic: The aggregation (grouping together) of two or more diseases or health conditions in a population in which there is some level of harmful biological or behavioral interface that exacerbates the negative health effects of any or all of the diseases involved. Syndemics involve the adverse interaction of diseases of all types, including infections, chronic non-communicable diseases, mental health problems, behavioral conditions, toxic exposure, and malnutrition.
Vector-borne diseases: Human illnesses caused by parasites, viruses, and bacteria that are transmitted by mosquitoes, flies, ticks, mites, snails, and lice.
Zoonoses: Diseases that can be transmitted from animals to humans.
About the Author
Joylin Namie
Truckee Meadows Community College, jnamie@tmcc.edu

Dr. Joylin Namie teaches courses in biological and cultural anthropology at Truckee Meadows Community College. Her research interests are in the areas of food, gender, media, and health. She began her career interviewing women in Costa Rica regarding beliefs about breast cancer and investigating the ways these affected engagement with cancer screening. She then moved to food studies, publishing on a variety of topics, including the cultural reasons mothers feed their children junk food, how images of successful athletes are used to market unhealthy foods as “fuel” for athletic pursuits, and feminine representation in sports nutrition advertising. She enjoys collaborating with students, including exploring plastic surgery among Latter-day Saint (Mormon) women in Utah, which resulted in a documentary film and an article that won the award for best paper in Social Science from the Utah Academy of Sciences, Arts, and Letters. She also co-researched and co-authored an article with students on the ways Mormon masculinity promotes involvement with child-feeding. In addition to teaching and research, Dr. Namie’s favorite things in life are competing in sports and traveling, often with her dog, Brooklyn, who has run behind her mountain bike everywhere from Vermont to Vancouver Island.
For Further Exploration
Lents, Nathan H. 2018. Human Errors: A Panorama of Our Glitches, from Pointless Bones to Broken Genes. Boston: Houghton Mifflin Harcourt.
Stearns, Stephen C., and Jacob C. Koella, eds. 2008. Evolution in Health and Disease. Second Edition. United Kingdom: Oxford University Press.
Zuk, Marlene. 2013. Paleofantasy: What Evolution Really Tells Us About Sex, Diet, and How We Live. New York: W.W. Norton & Company.
References
Abid, Zaynah, Amanda J. Cross, and Rashmi Sinha. 2014. “Meat, Dairy, and Cancer.” The American Journal of Clinical Nutrition 100, Issue Supplement 1 (1): 386S–393S.
Akil, Luma, and H. Anwar Ahmad. 2011. “Relationships between Obesity and Cardiovascular Diseases in Four Southern States and Colorado.” Journal of Health Care for the Poor and Underserved 22 (Suppl. 4): 61–72.
Akinbami, Lara J., Alan E. Simon, and Lauren M. Rossen. 2016. “Changing Trends in Asthma Prevalence among Children.” Pediatrics 137 (1). doi:10.1542/peds.2015-2354.
Ali, Aus Tariq. 2014. “Reproductive Factors and the Risk of Endometrial Cancers.” International Journal of Gynecological Cancer 24 (3): 384–393.
American Heart Association. 2014. “Smoking & Cardiovascular Disease (Heart Disease).” Last modified February 17, 2014. https://docs.google.com/ document/d/1iMgccSz67i37839NhIAPGQlwsWA3VGtSKtejlrGN_LI/edit.
——— 2018. “Heart Disease and Stroke Statistics 2017 At-a-Glance.” Last modified January 31, 2018. https://healthmetrics.heart.org/wp-content/uploads/2018/02/At-A-Glance-Heart-Disease-and-Stroke-Statistics-2018.pdf.
American Psychiatric Association (APA). 2013. Diagnostic and Statistical Manual of Mental Disorder. Fifth Edition: DSM-5. Washington, DC: APA.
Andrews, Tessa M., Steven T. Kalinowski, and Mary J. Leonard. 2011. “Are Humans Evolving? A Classroom Discussion to Change Students’ Misconceptions Regarding Natural Selection.” Evolution: Education and Outreach 4 (3): 456–466.
Armelagos, George. 1990. “Health and Disease in Populations in Transition.” In Disease in Populations in Transition, edited by Alan C. Swedlund and George J. Armelagos, 127–144. New York: Bergin & Garvey.
Armelagos, George J., Peter J. Brown, and Bethany Turner. 2005. “Evolutionary, Historical and Political Economic Perspectives on Health and Disease.” Social Science and Medicine 61 (4): 755–765.
Asher, Claire. 2017. “Illegal Bushmeat Trade Threatens Human Health and Great Apes.” Mongabay, April 6. https://news.mongabay.com/2017/04/illegal-bushmeat-trade-threatens-human-health-and-great-apes/.
Baer, Hans, and Merrill Singer. 2009. Global Warming and the Political Ecology of Health: Emerging Crises and Systemic Solutions. Walnut Creek, CA: Left Coast Press.
Baker, W.A., G.A. Hitman, K. Hawrami, M.I. McCarthy et al. 1994. “Apolipoprotein D Gene Polymorphism: A New Genetic Marker for Type 2 Diabetic Subjects in Nauru and South India.” Diabetic Medicine 11 (10): 947–952.
Baltic, Milan Z., and Marija Boskovic. 2015. “When Man Met Meat: Meat in Human Nutrition from Ancient Times Till Today.” Procedia Food Science 5: 6–9.
Beasley, Richard, Alex Semprini, and Edwin A. Mitchell. 2015. “Risk Factors for Asthma: Is Prevention Possible?” The Lancet 386 (9998): 1075–1085.
Berenbaum, Francis. 2011. “Diabetes-induced Osteoarthritis: From a New Paradigm to a New Phenotype.” Annals of the Rheumatic Diseases 70 (8). doi:10.1136/ard.2010.146399.
Berna, Francesco, Paul Goldberg, Liora Kolska Horwitz, James Brink, Sharon Holt, Marion Bamford, and Michael Chazan. 2012. “Microstratigraphic Evidence of In Situ Fire in the Acheulean Strata of Wonderwerk Cave, Northern Cape Province, South Africa.” Proceedings of the National Academy of Sciences 109: E1215e-E1220.
Blue Cross Blue Shield Association (BCBSA). 2017. “Diabetes and the Commercially Insured U.S. Population.” The Health of America Report, August 1. https://www.bcbs.com/the-health-of-america/reports/diabetes-and-commercially-insured-us-population.
Bogin, Barry. 1991. “The Evolution of Human Nutrition.” In The Anthropology of Medicine: From Culture to Method, edited by Lola Romanucci-Ross, Daniel E. Moerman, and Laurence R. Tancredi, 158–195. New York: Bergin & Garvey.
Bouchard, Claude. 2007. “The Biological Predisposition to Obesity: Beyond the Thrifty Genotype Scenario.” International Journal of Obesity 31: 1337–1339.
Brown, Peter J. 1991. “Culture and the Evolution of Obesity.” Human Nature 2 (1): 31–57.
Bruni, L., L. Barrionuevo-Rosas, G. Albero, B. Serrano et al. 2017. “Human Papillomavirus and Related Diseases in the World.” Summary Report 27, July. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). http://www.hpvcentre.net/statistics/reports/XWX.pdf.
Buchman, Aron S., Lei Yu, Robert S. Wilson, Andrew Lim, Robert J. Dawe, Chris Gaiteri, Sue E. Leurgans, Julie A. Schneider, and David A. Bennett. 2019. “Physical Activity, Common Brain Pathologies, and Cognition in Community-Dwelling Older Adults.” Neurology 98 (2). doi:10.1212/WNL.0000000000006954.
Center for Science in the Public Interest (CSPI). 2010. Food Dyes: A Rainbow of Risk. Washington, DC: Center for Science in the Public Interest.
Centers for Disease Control and Prevention (CDC). 2014. Breastfeeding Report Card: United States/2014. Atlanta, GA: Centers for Disease Control and Prevention.
———. 2016. “Leading Causes of Death.” National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm.
——— 2017. “Human Papillomavirus.” Genital HPV Infection—Fact Sheet. Atlanta, GA: Centers for Disease Control and Prevention.
———. 2017. “Asthma.” National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/asthma.htm.
Cerón, Ella. 2017. “Here’s Every Oreo Flavor Ever Created.” TeenVogue.com, June 19. https://www.teenvogue.com/story/every-oreo-flavor-ranked.
Chen, Yang, Yi-Lun Lee, and Guang-Hui Dong. 2012. “Gender Difference of Childhood Overweight and Obesity in Predicting the Risk of Incident Asthma: A Systematic Review and Meta-Analysis.” Obesity Reviews 14 (3): 222–231. doi:10.1111/j.1467-789X.2012.01055.x
Chin, Jessie, Brennan R. Payne, Wai-Tat Fu, Daniel G. Morrow, and Elizabeth A. L. Stine-Morrow. 2015. “Information Foraging across the Life Span: Search and Switch in Unknown Patches.” Topics in Cognitive Science 7 (3): 428–450.
Cooling, Laura. 2015. “Blood Groups in Infection and Host Susceptibility.” Clinical Microbiology Reviews 28 (3): 801–870.
Cordain, Loren. 2002. The Paleo Diet: Lose Weight and Get Healthy by Eating the Food You Were Designed to Eat. Hoboken, NJ: John Wiley & Sons.
Crosby, Alfred W., Jr. 2003. The Columbian Exchange: Biological and Cultural Consequences of 1492. 30th Anniversary Edition. Westport, CT: Praeger Publishers.
Croston, Glenn. 2012. “The Thing We Fear More Than Death: Why Predators Are Responsible for Our Fear of Public Speaking.” Psychology Today blog, November 29. https://www.psychologytoday.com/us/blog/the-real-story-risk/201211/the-thing-we-fear-more-death.
Crow, James F., and Motoo Kimura. 1970. An Introduction to Population Genetics Theory. New York: Harper and Row.
Currie, Candace, Naman Ahluwalia, Emmanuelle Godeau, Saoirse Nic Gabhainn, Pernille Due, and Dorothy B. Mille . 2012. “Is Obesity at Individual and National Level Associated with Lower Age at Menarche? Evidence from 34 Countries in the Health Behaviour in School-Aged Children Study.” Journal of Adolescent Health 50 (6): 621–626.
David, A. Rosalie, and Michael Zimmerman. 2010. “Cancer: An Old Disease, A New Disease or Something In Between?” Nature Reviews: Cancer 10 (10): 728–733.
Davis, Mike. 2005. The Monster at Our Door: The Global Threat of Avian Flu. New York: Owl Books.
de Silva, A. M., K. R. Walder, T. J. Aitman, T. Gotoda, A. P. Goldstone, A. M. Hodge, M. P. de Courten, P. Z. Zimmet, and G. R. Collier. 1999. “Combination of Polymophisms in OB-R and the OB Gene Associated with Insulin Resistance in Nauruan Males.” International Journal of Obesity 23 (8): 816–822.
Devuyst, Olivier. 2014. “High Time for Human Height.” Peritoneal Dialysis International 34 (7): 685–686.
Diamond, Jared. 1987. “The Worst Mistake in the History of the Human Race.” Discover, May: 64–66.
———. 1997. Guns, Germs, and Steel: The Fates of Human Societies. New York: W. W. Norton.
Dimsdale, Joel E. 2008. “Psychological Stress and Cardiovascular Disease.” Journal of the American College of Cardiology 51 (13): 1237–1246.
Dunn, Robb. 2018. Never Home Alone: From Microbes to Millipedes, Camel Crickets, and Honeybees, the Natural History of Where We Live. New York: Basic Books.
Dutton, Denis. 2009. The Art Instinct: Beauty, Pleasure, and Human Evolution. New York: Bloomsbury.
Eaton, S. Boyd, Melvin Konner, and Marjorie Shostak. 1988. “Stone Agers in the Fast Lane: Chronic Degenerative Diseases in Evolutionary Perspective.” American Journal of Medicine 84 (4): 739–749.
Eaton, S. Boyd, Malcolm C. Pike, Roger V. Short, Nancy C. Lee, James Trussell, Robert A. Hatcher, James W. Wood, et al. 1994. “Women’s Reproductive Cancers in Evolutionary Context.” The Quarterly Review of Biology 69 (3): 353–367.
Ewald, Paul W. 2018. “Ancient Cancers and Infection-Induced Oncogenesis.” International Journal of Paleopathology 21: 178–185. http://dx.doi.org/10.1016/J.ijpp.2017.08.007.
Fall, Tove, Cecilia Lundholm, Anne K. Orkqvist, Katja Fall et al. 2015. Early Exposure to Dogs and Farm Animals and the Risk of Childhood Asthma. JAMA Pediatrics 169 (11). doi: 10.1001/jamapediatrics.2015.3219.
Farb, Peter, and George Armelagos. 1980. Consuming Passions: The Anthropology of Eating. New York: Washington Square Press.
Findley, Sally, Katherine Lawler, Monisha Bindra, Linda Maggio, Madeline M. Penachio, and Christopher Maylahn. 2003. “Elevated Asthma and Indoor Environmental Exposures among Puerto Rican Children of East Harlem.” Journal of Asthma 40 (5): 557–569.
Flinn, Mark V., and Barry G. England. 2003. “Childhood Stress: Endocrine and Immune Responses to Psychosocial Events.” In Social and Cultural Lives of Immune Systems: Theory and Practice in Medical Anthropology and International Health, edited by James M. Wilce Jr., 105–146. London: Routledge.
Fumagalli, Matteo, Ida Moltke, Niels Grarup, Fernando Racimo, Peter Bjerregaard, Marit E. Jørgensen, Thorfinn S. Korneliussen, et al. 2015. “Greenlandic Inuit Show Genetic Signatures of Diet and Climate Adaptation.” Science349 (6254): 1343–1347.
Gao, George. 2015. “Americans’ Ideal Family Size Is Smaller Than It Used to Be.” Pew Research Center, May 8. http://www.pewresearch.org/fact-tank/2015/05/08/ideal-size-of-the-american-family/.
Gladwell, Malcolm. 2007. Blink: The Power of Thinking Without Thinking. New York: Back Bay Books.
Goulder, Philip J., Sharon R. Lewin, and Ellen M. Leitman. 2016. “Paediatric HIV Infection: The Potential for Cure.” Nature Reviews Immunology 16: 259–271.
Graber, Cynthia. 2014. “Michael Pollan Explains What’s Wrong with the Paleo Diet.” Mother Jones, January 17. https://www.motherjones.com/environment/2014/01/michael-pollan-paleo-diet-inquiring-minds/.
Greaves, Mel. 2015. “Evolutionary Determinants of Cancer.” Cancer Discovery 5 (8): 806–820.
Greenspan, Louise, and Julianna Deardorff. 2014. The New Puberty: How to Navigate Early Development in Today’s Girls. New York: Rodale.
Guadagno, Rosanna E., Bradley M. Okdie, and Sara A. Kruse. 2012. “Dating Deception: Gender, Online Dating, and Exaggerated Self-Presentation.” Computers in Human Behavior 28 (2): 642–647.
Guilak, Farshid. 2012. “Biomechanical Factors in Osteoarthritis.” Best Practice & Research: Clinical Rheumatology 25 (6): 815–823.
Gurven, Michael, and Hillard Kaplan. 2007. “Longevity among Hunter-Gatherers: A Cross-Cultural Examination.” Population and Development Review 33 (2): 321–365.
Hamilton, Cheryl. 2011. Communicating for Results, a Guide for Business and the Professions, Ninth Edition. Belmont, CA: Thomson Wadsworth.
Harper, Kristin, and George Armelagos. 2010. “The Changing Disease-Scape in the Third Epidemiological Transition.” International Journal of Environmental Research and Public Health 7 (2): 675–697.
Harris, Marvin. 1989. “Life Without Chiefs.” New Age Journal, November/December: 42–45, 205–209.
Hatton, Tim. 2014. “Why Did Humans Grow Four Inches in 100 Years? It Wasn’t Just Diet.” The Conversation, May 1. https://theconversation.com/why-did-humans-grow-four-inches-in-100-years-it-wasnt-just-diet-25919.
Hays, J. N. 2005. Epidemics and Pandemics: Their Impacts on Human History. Santa Barbara, CA: ABC-CLIO, Inc.
International Diabetes Federation (IDF). 2018. IDF Diabetes Atlas. Eighth Edition. http://www.diabetesatlas.org/key-messages.html.
Issa, Rital, and Timothy M. Griffin. 2012. “Pathobiology of Obesity and Osteoarthritis: Integrating Biomechanics and Inflammation.” Pathobiology of Aging and Age-Related Diseases 2 (1). https://doi.org/10.3402/pba.v2i0.17470.
Jain, H. K.. 2012. “Transition to Twenty-First Century Agriculture: Change of Direction.” Agricultural Research 1 (1): 12–17.
Jones, Kate E., Nikkita G. Patel, Mark A. Levy, Adam Storeygard, Deborah Balk, John L. Gittleman, and Peter Daszak. 2008. “Global Trends in Emerging Infectious Disease.” Nature 451 (7181): 990–993.
Jones, Rachel K., and Joerg Dreweke. 2011. Countering Conventional Wisdom: New Evidence on Religion and Contraceptive Use. Report, April 2011. New York: Guttmacher Institute.
Joseph, Christine L. M., Betsy Foxman, Frederick E. Leickly, Edward Peterson, and Dennis Ownby. 1996. “Prevalence of Possible Undiagnosed Asthma and Associated Morbidity among Urban Schoolchildren.” Journal of Pediatrics 129 (5): 735–742.
Kaczmarczyk, Melissa M., Michael J. Miller, and Gregory G. Freund. 2012. “The Health Benefits of Dietary Fiber: Beyond the Usual Suspects of Type 2 Diabetes Mellitus, Cardiovascular Disease and Colon Cancer.” Metabolism: Clinical and Experimental 61 (8): 1058–1066.
Larsen, Clark Spencer. 2014. “Foraging to Farming Transition: Global Health Impacts, Trends, and Variation.” In Encyclopedia of Global Archaeology, edited by Claire Smith, 2818–2824. New York: Springer.
Lattimer, James M., and Mark D. Haub. 2010. “Effects of Dietary Fiber and Its Components on Metabolic Health.” Nutrients 2 (12): 1266–1289.
Lee, Richard B. 2013. The Dobe Ju/’hoansi. Fourth Edition. Belmont, CA: Wadsworth/Cengage Learning.
Leontis, Lisa M. N.d. “Type 2 Diabetes and Exercise: Exercise Makes It Easier to Control Your Diabetes.” https://www.endocrineweb.com/conditions/type-2-diabetes/type-2-diabetes-exercise.
Lieberman, Daniel E. 2015. “Human Locomotion and Heat Loss: An Evolutionary Perspective.” Comprehensive Physiology 5(1): 99–117.
Lieberman, Leslie Sue. 2006. “Evolutionary and Anthropological Perspectives on Optimal Foraging in Obesogenic Environments.” Appetite 47 (1): 3–9.
Liu, Gang. 2018. “Abstract P184: Meat Cooking Methods and Risk of Hypertension: Results From Three Prospective Cohort Studies.” Circulation 137 (Suppl. 1): AP184.
Liu, Gang, Geng Zong, Kana Wu, Yang Hu, Yanping Li, Walter C. Willett, David M. Eisenberg, Frank B. Hu, and Qi Sun. 2018. “Meat Cooking Methods and Risk of Type 2 Diabetes: Results From Three Prospective Cohort Studies.” Diabetes Care 41 (5): 1049–1060.
Livingston, Gretchen. 2015. “Childlessness.” Pew Research Center, May 7. http://www.pewsocialtrends.org/2015/05/07/childlessness/.
Lopalco, Lucia. 2010. “CCR5: From Natural Resistance to a New Anti-HIV Strategy.” Viruses 2 (2): 574–600.
Lucock, Mark D., Charlotte E. Martin, Zoe R. Yates, and Martin Veysey. 2014. “Diet and Our Genetic Legacy in the Recent Anthropocene: A Darwinian Perspective to Nutritional Health.” Journal of Evidence-Based Complementary and Alternative Medicine 19 (1): 68–83.
Main, Douglas. 2013. “Ancient Mutation Explains Missing Wisdom Teeth.” Live Science, March 13. https://www.livescience.com/27529-missing-wisdom-teeth.html.
Malina, Robert M., and Bertis B. Little. 2008. “Physical Activity: The Present in the Context of the Past.” American Journal of Human Biology 20 (4): 373–391.
Mandsager, Kyle, Serge Harb, and Paul Cremer. 2018. “Association of Cardiorespiratory Fitness with Long-term Mortality among Adults Undergoing Exercise Treadmill Testing.” JAMA Network Open 1 (6): e183605. doi:10.1001/jamanetworkopen.2018.3605.
Marciniak, Stephanie, and George H. Perry. 2017. “Harnessing Ancient Genomes to Study the History of Human Adaptation.” Nature Reviews Genetics 18: 659–674.
Marlowe, Frank W. 2005. “Hunter-Gatherers and Human Evolution.” Evolutionary Anthropology 14 (2): 54–67.
Marmot, Michael. 2005. “Social Determinants of Health Inequality.” The Lancet 365 (9464): 1099–1104.
Martini, Frederic H., William C. Ober, Edwin F. Bartholomew, and Judi L. Nath. 2013. Visual Essentials of Anatomy & Physiology. Boston, MA: Pearson.
Mathews, T.J., and Brady E. Hamilton. 2016. “Mean Age of Mothers Is on the Rise: United States, 2000–2014.” National Center for Health Statistics (CHS) Data Brief. No. 232. https://www.cdc.gov/nchs/data/databriefs/db232.pdf.
McElroy, Ann, and Patricia Townsend. 2009. Medical Anthropology in Ecological Perspective. Fifth Edition. Boulder, CO: Westview Press.
McEvoy, Claire T., Norman Temple, and Jayne V. Woodside. 2012. “Vegetarian Diets, Low-Meat Diets and Health: A Review.” Public Health Nutrition 15 (12): 2287–2294.
McKee, Trudy, and James R. McKee. 2015. Biochemistry: The Molecular Basis of Life. Sixth Edition. Oxford, UK: Oxford University Press.
Moss, Michael. 2013. Salt, Sugar, Fat: How the Food Giants Hooked Us. New York: Random House.
National Geographic Society. N.d. Resource Library: Encyclopedic Entry (n.d.), s.v., “Autotroph.” National Geographic Society. https://www.nationalgeographic.org/encyclopedia/autotroph/.
National Institutes of Health (NIH). 2017. “Obesity and Cancer Fact Sheet.” Last modified January, 2017. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/obesity-fact-sheet.
Neeha, V. S., and Priyamvadah Kinth. 2013. “Nutrigenomics Research: A Review.”Journal of Food Science and Technology, 50 (3): 415–428.
Neel, James V. 1962. “Diabetes Mellitus: A ‘Thrifty’ Genotype Rendered Detrimental by ‘Progress’?” American Journal of Human Genetics 14 (4): 353–362.
Novembre, John, Alison P. Galvani, and Montgomery Slatkin. 2005. “The Geographic Spread of the CCR5 Δ32 HIV-Resistance Allele.” PLoS Biology 3 (11): e339.
Odes, Edward J., Patrick S. Randolph-Quinney, Maryna Steyn, Zach Throckmorton, Jacqueline S. Smilg, Bernhard Zipfel, Tanya N. Augustine, et al. 2016. “Earliest Hominin Cancer: 1.7-Million-Year-Old Osteosarcoma from Swartkrans Cave, South Africa.” South African Journal of Science 112 (7–8): 1–5.
O’Keefe Osborn, Corinne. 2017. “Type 1 and Type 2 Diabetes: What’s the Difference?” Healthline Newsletter, August 24. https://www.healthline.com/health/Difference-between-type-1-and-type-2-diabetes.
Omran, Abdel R. 1971. “The Epidemiological Transition: A Theory of the Epidemiology of Population Change.” Milbank Memorial Fund Quarterly 49 (4): 509–538.
———. 2005. “The Epidemiological Transition: A Theory of the Epidemiology of Population Change.” The Milbank Quarterly 83 (4): 731–757.
Organ, Chris, Charles L. Nunn, Zarin Machanda, and Richard W. Wrangham. 2011. “Phylogenetic Rate Shifts in Feeding Time during the Evolution of Homo.” Proceedings of the National Academy of Sciences 108 (35): 14555–14559.
Ortega, Alexander Neil, Peter J. Gergen, A. David Paltiel, Howard Bauchner, Kathleen D. Belanger, and Brian P. Leaderer. 2002. “Impact of Site of Care, Race, and Hispanic Ethnicity on Medication Use for Childhood Asthma.” Pediatrics 109 (1): E1.
Palma-Gudiel, H., A. Córdova-Palomera, E. Eixarch, M. Deuschle, and L. Fañanás. 2015. “Maternal Psychosocial Stress during Pregnancy Alters the Epigenetic Signature of the Glucocorticoid Receptor Gene Promoter in Their Offspring: A Meta-Analysis.” Epigenetics 10 (10): 893–902.
Pamuk, Şevket. 2007. “The Black Death and the Origins of the ‘Great Divergence’ across Europe, 1300–1600.” European Review of Economic History 11 (3): 289–317.
Pearl, Robert. 2015. “Why Health Care Is Different if You’re Black, Latino, or Poor.” Forbes, March 5. https://www.forbes.com/sites/robertpearl/2015/03/05/healthcare-black-latino-poor/#1ab6e3807869.
Physical Activity Council. 2018. 2018 Participation Report. http://www.physicalactivitycouncil.com/pdfs/current.pdf.
Pickering, Travis Rayne, and Henry T. Bunn. 2007. “The Endurance Running Hypothesis and Hunting and Scavenging in Savanna-Woodlands.” Journal of Human Evolution 53 (4): 434–438.
Pierce, Mary, and Rebecca Hardy. 2012. “Commentary: The Decreasing Age of Puberty— As Much a Psychosocial as Biological Problem?” International Journal of Epidemiology 41 (1): 300–302.
Plotnikoff, Ronald C., Sarah A. Costigan, Rebecca L. Williams, Melinda J. Hutchesson, Sarah G. Kennedy, Sara L. Robards, Jennifer Allen, Clare E. Collins, Robin Callister, and John Germov. 2015. “Effectiveness of Interventions Targeting Physical Activity, Nutrition and Healthy Weight for University and College Students: A Systematic Review and Meta-analysis.” International Journal of Behavioral Nutrition and Physical Activity 12 (1): 1–10.
Poinar, George. 2018. “Vertebrate Pathogens Vectored by Ancient Hematophagous Arthropods.” Historical Biology, November 7. doi:10.1080/08912963.2018.1545018.
Pontzer, Herman, David A. Raichlen, Brian M. Wood, Audax Z. P. Mabulla, Susan B. Racette, and Frank W. Marlowe. 2012. “Hunter-Gatherer Energetics and Obesity.” PLoS ONE 7 (7): e40503. doi:10.1371/journal.pone.0040503.
Pritchard, Jonathan K. 2010. “How We Are Evolving.” Scientific American 303 (4): 4047.
Raichlen, David A., and Gene E. Alexander. 2014. “Exercise, APOE Genotype, and the Evolution of the Human Lifespan.” Trends in Neurosciences 37 (5): 247–255.
Raichlen, David A., Herman Pontzer, Jacob A. Harris, Audax Z. P. Mabulla, Frank W. Marlowe, J. Josh Snodgrass, Geeta Eick, J. Colette Berbesque, Amelia Sancilio, Brian M. Wood. 2016. “Physical Activity Patterns and Biomarkers of Cardiovascular Disease Risk in Hunter-Gatherers.” American Journal of Human Biology 29 (2): e22919. https://doi.org/10.1002/ajhb.22919.
Rankinen, Tuomo, Aamir Zuberi, Yvon C. Chagnon, S. John Weisnagel, George Argyropoulos, Brandon Walts, Louis Pérusse, and Claude Bouchard. 2006. “The Human Obesity Gene Map: The 2005 Update.” Obesity 14 (4): 529–644.
Richards, M. P. 2002. “A Brief Review of the Archaeological Evidence for Palaeolithic and Neolithic Subsistence.” European Journal of Clinical Nutrition 56 (12): 1270–1278.
Sallis, James F., Neville Owen, and Edwin B. Fisher. 2008. “Chapter 20: Ecological Models of Health Behavior.” In Health Behavior and Health Education: Theory, Research, and Practice, edited by Karen Glanz, Barbara K. Rimer, and K. Viswanath, 465–485. Fourth Edition. San Francisco, CA: Jossey-Bass.
Sharp, Paul M., and Beatrice H. Hahn. 2011. “Origins of HIV and the AIDS Pandemic.” Cold Springs Harbor Perspectives in Medicine 1 (1): a006841.
Shreiner, Andrew B., John Y. Kao, and Vincent B. Young. 2015. “The Gut Microbiome in Health and Disease.” Current Opinion in Gastroenterology 31 (1): 69–75.
Singer, Merrill, and Hans Baer. 2012. “Health Disparity, Health Inequality.” In Introducing Medical Anthropology: A Discipline in Action, Second edition, edited by Merrill Singer and Hans Baer, 175–205. Lanham, MD: AltaMira.
Singer, Merrill, and Scott Clair. 2003. “Syndemics and Public Health: Reconceptualizing Disease in Bio-Social Context.” Medical Anthropology Quarterly 17 (4): 423–441.
Singer, Merrill, Nicola Bulled, Bayla Ostrach, and Emily Mendenhall. 2017. “Syndemics and the Biosocial Conception of Health.” Lancet 389 (10072): 941–950.
Small, Meg, Lisa Bailey-Davis, Nicole Morgan, and Jennifer Maggs. 2013. “Changes in Eating and Physical Activity Behaviors across Seven Semesters of College: Living On or Off Campus Matters.” Health Education and Behavior 40 (4): 435–441.
Smith-Morris, Carolyn M. 2004. “Reducing Diabetes in Indian Country: Lessons from the Three Domains Influencing Pima Diabetes.” Human Organization 63 (1): 34–46.
Sonfield, Adam, Kinsey Hasstedt, Megan L. Cavanaugh, and Ragnar Anderson. 2013. The Social and Economic Benefits of Women’s Ability to Determine Whether and When to Have Children. New York: Guttmacher Institute. https://www.guttmacher.org/report/social-and-economic-benefits-womens-ability-determine-whether-and-when-have-children.
Stearns, Stephen C., Randolph M. Nesse, and David Haig. 2008. “Introducing Evolutionary Thinking into Medicine.” In Evolution in Health and Disease, edited by Stephen C. Stearns and Jacob C. Koella, 3–15. United Kingdom: Oxford University Press.
St. Pierre, Danielle. 2018. “The 15 Best Potato Chips for Every Flavor Craving.” Best, April 6. Retrieved June 13, 2018 from https://www.bestproducts.com/eats/food/g972/best-potato-chips/.
Strassmann, Beverly I. 1997. “The Biology of Menstruation in Homo Sapiens: Total Lifetime Menses, Fecundity, and Nonsynchrony in a Natural-Fertility Population.” Current Anthropology 38 (1): 123–129.
———. 1999. “Menstrual Cycling and Breast Cancer: An Evolutionary Perspective.” Journal of Women’s Health 8 (2): 193–202.
Tierney, Mike. 2013. “At Spelman, Dropping Sports in Favor of Fitness.” New York Times, April 13. https://www.nytimes.com/2013/04/14/sports/at-spelman-dropping-sports-in-favor-of-fitness.html.
Trafialek, Joanna, and Wojciech Kolanowski. 2014. “Dietary Exposure to Meat-Related Carcinogenic Substances: Is There a Way to Estimate the Risk?” International Journal of Food Sciences and Nutrition 65 (6): 774–780.
UNAIDS. 2018. “Fact Sheet: Latest Statistics on the AIDS Epidemic.” http://www.unaids.org/en/resources/fact-sheet.
Ventola, C. Lee. 2015. “The Antibiotic Resistance Crisis: Part I: Causes and Threats.” Pharmacy & Therapeutics 40 (4): 277–283.
Versini, M., Jeandel, P., Bashi, T., Bizzaro, G., Blank, M., and Shoenfeld, Y. 2015. “Unraveling the Hygiene Hypothesis of Helminthes and Autoimmunity: Origins, Pathophysiology, and Clinical Applications.” BMC Medicine, 13: 81. https://doi.org/10.1186/s12916-015-0306-7.
Vucenik, Ivana, and Joseph P. Stains. 2012. “Obesity and Cancer Risk: Evidence, Mechanisms, and Recommendations.” Special issue, “Nutrition and Physical Activity in Aging, Obesity, and Cancer,” Annals of the New York Academy of Sciences Volume 1271:: 37–43.
Walker, Polly, Pamela Rhubart-Berg, Shawn McKenzie, Kristin Kelling, and Robert S. Lawrence. 2005. “Public Health Implications of Meat Production and Consumption.” Public Health Nutrition 8 (4): 348–356.
Washington, Jesse. 2010. “Blacks Struggle with 72% Unwed Mothers Rate.” NBCNEWS.com, November 7. http://www.nbcnews.com/id/39993685/ns/health-womens_health/t/blacks-struggle-percent-unwed-mothers-rate/#.XEETH89KjBJ.
Willett, Walter, Johan Rockström, Brent Loken, Marco Springmann, Tim Lang, Sonja Vermeulen, Tara Garnett, et al. 2019. “Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems.” The Lancet, January 16. http://dx.doi.org/10.1016/S0140-6736(18)31788-4.
Williams, David R., and Selina A. Mohammed. 2013. “Racism and Health I: Pathways and Scientific Evidence.” American Behavioral Scientist 57 (8). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3863357/.
Wolfe, Nathan, Claire P. Dunavan, and Jared Diamond. 2012. “Origins Of Major Human Infectious Diseases.” In Institute of Medicine: Improving Food Safety Through a One Health Approach: Workshop Summary. Washington, DC: National Academies Press. A16. https://www.ncbi.nlm.nih.gov/books/NBK114494/.
Woo, Kam S., Timothy C.Y. Kwok, and David S. Celermajer. 2014. “Vegan Diet, Subnormal Vitamin B-12 Status and Cardiovascular Health.” Nutrients 6 (8): 3259–3273.
World Health Organization (WHO). 2016. Global Report on Diabetes. http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf.
———. 2017a. “Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016.” Geneva: WHO.
———. 2017b. “Obesity and Overweight.” Fact Sheet. Last modified October 2017. http://www.who.int/mediacentre/factsheets/fs311/en/.
———. 2018a. Global Health Observatory (GHO) Data. “Life Expectancy.” http://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends/en.
———. 2018b. “Cancer.” Fact Sheet. Last modified February 2018. http://www.who.int/news-room/fact-sheets/detail/cancer.
———. 2018c. “Healthy Diet.” Fact Sheet. Last modified October 2018. https://www.who.int/news-room/fact-sheets/detail/Healthy-diet.
———. n.d. “Influenza.” Accessed January 7, 2019 from https://www.who.int/influenza/human_animal_interface/avian_influenza/h5n1_research/faqs/en/.
Worthman, Carol M., and Jennifer Kuzara. 2005. “Life History and the Early Origins of Health Differentials.” American Journal of Human Biology 17 (1): 95–112.
Wrangham, Richard. 2009. Catching Fire: How Cooking Made Us Human. New York: Basic Books.
Yehuda, Rachel, and Joseph LeDoux. 2007. “Response Variation Following Trauma: A Translational Neuroscience Approach to Understanding PTSD.” Neuron 56 (1): 19–32.
Zuckerman, Molly K., and George J. Armelagos. 2014. “The Hygiene Hypothesis and the Second Epidemiologic Transition.” In Modern Environments and Human Health: Revisiting the Second Epidemiologic Transition, edited by Molly K. Zuckerman, 301-320. Hoboken, NJ: Wiley-Blackwell.
Zuckerman, Molly Kathleen, Kristin Nicole Harper, Ronald Barrett, and George John Armelagos. 2014. “The Evolution of Disease: Anthropological Perspectives on Epidemiologic Transitions.” Special issue, “Epidemiological Transitions: Beyond Omran’s Theory,” Global Health Action 7(1): 23303. doi:10.3402/gha.v7.23303.
Zuk, Marlene. 2013. Paleofantasy: What Evolution Really Tells Us About Sex, Diet, and How We Live. New York: W. W. Norton.
Figure Attributions
Figure 16.1 Carcinogenic Meats a derivative work original to Explorations: An Open Invitation to Biological Anthropology by Katie Nelson is under a CC BY-NC 4.0 License. [Includes Hot dog PNG image by unknown, CC BY-NC 4.0; Rasher of Bacon by unknown, public domain (CC0); Salami aka by André Karwath Aka, CC BY-SA 2.5; Cow PNG image by unknown, CC BY-NC 4.0; sheep PNG image by unknown, CC BY-NC 4.0; Pig on white background by unknown, public domain (CC0).]
Figure 16.2 Hadazbe returning from hunt by Andreas Lederer has been modified (cropped) and is used under a CC BY 2.0 License.
Figure 16.3 Obesity rates by country original to Explorations: An Open Invitation to Biological Anthropology by Katie Nelson is under a CC BY-NC 4.0 License. Based on data from Obesity Update. 2017. Organisation for Economic Co-operation and Development (OECD) Health Statistics.
Figure 16.4 The potato in three modern forms a derivative work original to Explorations: An Open Invitation to Biological Anthropology by Joylin Namie and Katie Nelson is under a CC BY-NC 4.0 License. [Includes Potato by unknown, public domain (CC0); McDonalds-French-Fries-Plate by Evan-Amos, public domain (CC0); Potato chips bowl by unknown, public domain (CC0).]
Figure 16.5 Participants of a walk against Diabetes and for general fitness around Nauru airport by Lorrie Graham, Department of Foreign Affairs and Trade is used under a CC BY 2.0 License.
Figure 16.6 Medical complications of obesity by the Centers for Disease Control and Prevention (CDC) is in the public domain.
Figure 16.7 Glucose metabolism original to Explorations: An Open Invitation to Biological Anthropology by Mary Nelson is under a CC BY-NC 4.0 License.
Figure 16.8 Type 1 and Type 2 Diabetes original to Explorations: An Open Invitation to Biological Anthropology by Mary Nelson is under a CC BY-NC 4.0 License.
Figure 16.9 Top ten causes of death in the U.S. and worldwide original to Explorations: An Open Invitation to Biological Anthropology by Joylin Namie is under a CC BY-NC 4.0 License. Based on data from Centers for Disease Control and Prevention (2016) and World Health Organization (2018).
Figure 16.10 Map of CCR5-delta32 allele distribution original to Explorations: An Open Invitation to Biological Anthropology by Katie Nelson is under a CC BY-NC 4.0 License. [Includes Europe Map Western Political 32847, unknown, Pixabay License; data from Solloch, Ute V., Kathrin Lang, Vinzenz Lange, and Irena Böhme. 2017. “Frequencies of gene variant CCR5-Δ32 in 87 countries based on next-generation sequencing of 1.3 million individuals sampled from 3 national DKMS donor centers.” Human Immonology, 78 (11-12).]
Figure 16.11 HIV-world-map-UNAIDS by UNAIDS has been designated to the public domain (CC0).
Figure 16.12 Row four man woman people walking together 3755342 by MaxPixel has been designated to the public domain (CC0).
The number of cases of disease per unit of population occurring over a unit of time.
The number of deaths attributable to a particular cause per unit of population over a unit of time.
A transformation in patterns of disease (morbidity) and death (mortality) among a population.
A medical condition in which excess body fat has accumulated to the point that it has adverse effects on health. The most widely used measure for identifying obesity is the Body Mass Index (BMI), a person’s weight in kilograms divided by the square of their height in meters. A measure of 30 kg/m2 is considered obese and 25—29 kg/m2 overweight. Distribution of body fat also matters. Fat in the abdominal region has a stronger association with Type 2 diabetes and cardiovascular disease, meaning waist to hip ratio and waist circumference are also important indicators of obesity-related health risk.
Refers to the degeneration of joint cartilage and underlying bone, causing pain and stiffness. In the absence of previous injury, it is most common in modern populations from middle age onward.
A collection of related diseases in which some of the body’s cells begin to divide without stopping and spread into surrounding tissues.
Autotrophic organisms are capable of producing their own food using inorganic substances such as light, water, carbon dioxide or chemical energy.
Organisms whose diet consists of plant and animal matter.
High blood pressure. Blood pressure is the force exerted by the blood against the walls of the blood vessels. In a blood pressure reading, the top number (usually higher) refers to the systolic pressure, the amount of pressure in your arteries during the contraction of your heart muscle when your heart beats. The bottom number is the diastolic pressure when your heart muscle is resting between beats. Hypertension can lead to severe health complications and increases the risk of heart attack and stroke.
A cluster of conditions, including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels that occur together, increasing the risk of heart disease, stroke, and diabetes. Lifestyle changes like losing weight, regularly exercising, and making dietary changes can help prevent or reverse metabolic syndrome.
A disease of the heart and blood vessels, often related to atherosclerosis, CVD is a condition in which a substance called plaque builds up in the walls of the arteries, blood vessels that carry blood away from the heart, compromising the flow of blood to the heart or brain.
Diseases that can be transmitted from animals to humans.
Human illnesses caused by parasites, viruses, and bacteria that are transmitted by mosquitoes, flies, ticks, mites, snails, and lice.
Living in groups settled permanently in one place.
Also known as chronic diseases, NCDs tend to be of long duration and are the result of a combination of genetic, physiological, environmental, and behavior factors. The main types of NCDs are cardiovascular diseases (like heart attacks and stroke), cancers, chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma), and diabetes.
Refers to parts of the world in which there is a prevalence of chronic disease (e.g.,. cancer, heart disease) while, at the same time, there are also high rates of infectious disease due to poverty, malnutrition, poor sanitation, and lack of access to health care, often accompanied by high rates of maternal and child mortality.
Infections that have recently appeared within a population or those whose incidence or geographic range is rapidly increasing or threatens to increase in the near future. Examples include Ebola, Zika, SARS, and avian (bird) flu.
The proportion of individuals in a population who have a particular disease or condition at a given point in time.
Promoting excessive weight gain. For example, an environment in which tasty, cheap food filled with excess calories is abundant.
Those organs in the body whose primary function is the production of hormones.
A way of life characterized by much sitting and little physical activity.
A person’s weight in kilograms divided by the square of their height in meters. The most widely used measure for identifying obesity. The formula using kilograms and meters (or centimeters) is
A stroke occurs when a blood vessel leading to the brain is blocked or bursts, preventing that part of the brain from receiving blood and oxygen, leading to the death of cells in that part of the brain.
An endocrine disorder in which high glucose (blood sugar) levels occur over a prolonged period of time. Blood glucose is your body’s main source of energy and comes from the food you eat. Insulin, a hormone made by the pancreas, helps glucose from food get into your cells to be used for energy. Sometimes your body does not make enough—or any—insulin (Type 1 diabetes) or does not take up insulin well (Type 2 diabetes). Glucose then stays in your blood and does not reach your cells.
A hormone produced in the pancreas that regulates the amount of glucose in the blood. Lack of insulin or the inability to absorb insulin causes diabetes.
A system that ranks foods on a scale from 1 to 100 based on their effect on blood-sugar levels. Carbohydrates with a low GI value (55 or less) are more slowly digested and metabolised causing a lower, slower rise in blood glucose and insulin levels.
A predictable response to any significant threat to homeostasis. The human stress response involves the central nervous system and the endocrine system acting together. Sudden and severe stress incites the “flight or flight” response from the autonomic nervous system in conjunction with hormones secreted by the adrenal and pituitary glands, increasing our heart rate and breathing and releasing glucose from the liver for quick energy.
The rate at which new cases of a disease occur in a population over a given period of time.
The first occurrence of menstruation.
The complex of nerve tissues stemming from the brain and spinal cord that controls the activities of the body.
Those organs in the body whose primary function is the production of hormones.
The biological system that circulates blood around the body via the heart, arteries, and veins, delivering oxygen and nutrients to organs and cells and carrying waste products away.
The aggregation (grouping together) of two or more diseases or health conditions in a population in which there is some level of harmful biological or behavioral interface that exacerbates the negative health effects of any or all of the diseases involved. Syndemics involve the adverse interaction of diseases of all types, including infections, chronic non-communicable diseases, mental health problems, behavioral conditions, toxic exposure, and malnutrition.
Ecological models of health and disease emphasize environmental and policy contexts of behavior, while incorporating social and psychological influences, rather than focusing on individual behaviors. These models encompass multiple levels of influence and can lend themselves to more comprehensive health interventions.
