Anatomy and Physiology
16 Autonomic Nervous System
 Wai o kāunu.
Wai o kāunu.
Water of love.
The thrilling effects of being in love.
‘Ōlelo No‘eau, compiled by Mary Kawena Pukui, #2914
Introduction
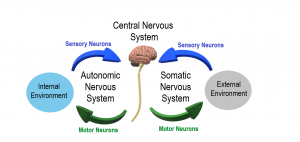
Figure 16.1: Autonomic Nervous System
![]() Chapter Learning Outcomes
Chapter Learning Outcomes
- Describe the components of the autonomic nervous system and understand how it is different from the somatic nervous system
- Understand the anatomy of the sympathetic and parasympathetic divisions of the autonomic nervous system
- Understand the neurotransmitters and receptors involved in preganglionic and postganglionic neurons of the autonomic nervous system.
- Learn about the reflexes of the autonomic nervous system and understand the concept of autonomic tone
- Know the organ-specific effects of sympathetic and parasympathetic stimulation
- Understand the inputs into the hypothalamus and understand how it regulates autonomic tone through control of both the sympathetic and parasympathetic divisions of the autonomic nervous system.
- Understand how sympathetic and parasympathetic agonist and antagonist drugs can be used to stimulate or inhibit organs controlled by the autonomic nervous system.
16.1 Autonomic Nervous System
![]() 16.1 Learning Outcomes
16.1 Learning Outcomes
- Understand the general structure of the autonomic nervous system
- Understand the concept of balance or homeostasis and how it is controlled through the two divisions of the autonomic nervous system.
- Compare and contrast the autonomic and somatic nervous systems
Have you ever noticed an incoming call from your ipo (Hawaiian for sweetheart), and before you even say hello, your heart is pounding so hard you can feel it in your chest?

Figure 16.2: Love is on the way. (Micah Camara, Flickr) CC-BY-NC-ND 2.0
Or perhaps you are on your scooter, and a car swerves into your lane. You feel the heat as you break out into a sweat. In both of those instances, you have activated the fight-or-flight pathways of the sympathetic nervous system, part of your autonomic nervous system. The other part of the autonomic nervous system (ANS) is the parasympathetic nervous system, which controls functions associated with rest-and-digest. Learning more about your ANS will give you insight into managing your stress responses to increase your health and make those responses work to your advantage. Many cultures from the ancients to the present day refer to the value of maintaining a balance between the sympathetic and s of the ANS as a part of optimal health. In Chinese medicine, the concept of the balance between postnatal qi and prenatal qi, and the associated disorder that results if the balance between them is lost, closely parallels that of the Western medicine model predicting disorders from lack of balance in the autonomic nervous system. For example, cardiovascular disease is associated with remaining too often in the fight or flight mode due to sustained stress. One quick way to shift away from that sympathetic state is to take three slow deep breaths. With each breath, expand the belly as you inhale. Then, hold your breath with the belly out for a moment before slowly exhaling and bringing the belly back to its resting position. The next time you sit down to take an anatomy and physiology exam, try taking those abdominal breaths, and feel your body shift from a sympathetic to parasympathetic dominant state.
Somatic versus autonomic
In the first half of this course, you learned about the somatic nervous system. Somatic motor neurons innervate skeletal muscles. For example, use your left hand to squeeze your right bicep while your arm is relaxed. You will notice that skeletal muscles are soft and limp when not activated. If you bend your elbow, flexing hard, you will activate your bicep, and it will feel firmer. Activating a somatic motor neuron excites the skeletal muscle leading to contraction. Somatic movements are also most often under conscious control. For example, you voluntarily decide to lift something heavy or move your leg. However, the somatic nervous system also generates involuntary responses, such as those associated with breathing, posture, balance, and es. In the somatic nervous system, the effector is always skeletal muscle, and the molecule released on the effector is always (ACh) which is always excitatory. The activation or input for the somatic nervous system includes voluntary signals from the cerebral cortex’s motor area and involuntary triggering of somatic reflexes by sensory neurons (somatic and special senses).
The ANS differs from the somatic nervous system in many ways. One is that its activation can lead to inhibition of an effector and excitation. Inhibition in this sense could be slowing the heart rate or reducing the release of digestive enzymes. Another difference is that the autonomic nervous system effectors are not skeletal muscles. Instead, they are cardiac muscle, smooth muscle, glands, and adipose tissue. Most ANS effectors are part of the body’s internal organs (viscera), so the effectors are usually called visceral effectors. Recall our examples at the beginning of the chapter: your heart started pounding because of your ipo’s phone call, and you started sweating when a car swerved in front of you. Pause a moment and imagine those scenarios. What are the effectors for increasing your heart’s force of contraction and making you sweat? Don’t read ahead until you have considered an answer. Did you say cardiac muscle and sweat glands? Correct!
 |
| Figure 16.3: Pathways of motor neurons in the somatic and autonomic nervous system showing cell body originating in the spinal cord, pathway, and effectors. |
 |
 |
| Figure 16.4: Autonomic Nervous System | Figure 16.5: Autonomic Nervous System Schematic Representation |

Figure 16.6: Somatic, Autonomic, and Enteric Structures of the Nervous System Somatic structures include the spinal nerves, both motor and sensory fibers, as well as the sensory ganglia (posterior root ganglia and cranial nerve ganglia). Autonomic structures are found in the nerves also, but include the sympathetic and parasympathetic ganglia. The enteric nervous system includes the nervous tissue within the organs of the digestive tract.

Figure 16.7: Autonomic Sympathetic Nerves: In response to stress, the hypothalamus (H) releases the corticotrophin releasing factor (CRF) into the anterior pituitary (P), causing the release of adrenocorticotropic hormone (ACTH) into the blood flow. ACTH stimulates the generation of glucocorticoids (cortisol in humans and corticosterone in mice) in the cortex of the adrenal gland (A), which are then released into the blood. Stress also activates the autonomic sympathetic nerves in the medulla of the adrenal gland to elicit the production of catecholamines, and , which are then released into the blood. Glucocorticoids and catecholamines influence the generation of interleukins, which are involved in the viability and proliferation of immunocompetent gut cells via receptors.

Figure 16.8: Adrenal Medulla: A flow diagram showing the process of stimulation of that makes it release adrenaline, that further acts on adrenoreceptors leading to increased sympathetic activity.

Figure 16.9: Connections of Parasympathetic Division of the Autonomic Nervous System Neurons from brain-stem nuclei, or from the lateral horn of the sacral spinal cord, project to near or within the various organs of the body. Axons from these s then project the short distance to those s.
| Somatic Nervous System | Autonomic Nervous System | |
| Input: | Somatic senses (touch, temp, pain, etc.), special senses (smell, taste, vision, etc.) | Interoceptors, somatic senses (touch, temp, pain, etc.), special senses (smell, taste, vision, etc.) |
| Output: | One neuron | Two neurons |
| Chemical signals: | Acetylcholine | Acetylcholine from preganglionic neuron; norepinephrine, acetylcholine from postganglionic neuron; norepinephrine, epinephrine from the adrenal gland |
| Effect: | Excitation | Inhibition or excitation |
| Effector: | Skeletal muscle | Cardiac muscle, smooth muscle, glands |
Table 16.1: Comparison of somatic and autonomic nervous systems
16.2 Anatomy of the Sympathetic and Parasympathetic Divisions of the Autonomic Nervous System
![]() 16.2 Learning Outcomes
16.2 Learning Outcomes
- Understand the concept of divergence and how it relates to a functional fight or flight response
- Understand the difference between preganglionic and postganglionic neurons
- Know the anatomy of the sympathetic nervous system
- Understand how the sympathetic nervous system activates the adrenal glands and why their activation is important in a fight or flight response
- Know the anatomy of the parasympathetic nervous system
- Understand what the enteric nervous system is and what it controls
The Sympathetic Division
The of the autonomic nervous system (ANS) has much more extensive divergence than the parasympathetic division. This allows us to respond rapidly to perceived danger. For example, you are surfing a large swell and the biggest set of the day starts heading your way. This would trigger several things to happen at the same time. In other words, the reflexive response would diverge or branch, allowing your response to be much more extensive than a simple somatic reflex. In this example, your pupils would dilate, your heart rate and blood pressure would go up, the blood vessels to the skeletal and cardiac muscles would vasodilate to deliver more blood, and the airways would dilate to allow you to bring in more oxygen to feed your muscles. Thanks to your courage and sympathetic nervous system, turn, paddle, and catch that wave. This is just a small sample of the many responses that would be initiated. Additionally, the adrenal gland would be stimulated to flood your system with adrenalin and stimulate widespread sympathetic responses. These things would happen quickly to allow you to deal with the perceived danger and prepare for a fight, flight…or surf.
The sympathetic nervous system (SNS) is sometimes referred to as the thoracolumbar division because the cell bodies of the preganglionic neurons are located in the lateral horn of the thoracic and first two lumbar spinal segments. The preganglionic neurons are relatively short and extend to postganglionic neurons in the nearby sympathetic chain (paravertebral) ganglia and collateral (prevertebral) ganglia (see image). The in the chain run next to the spinal cord on the left and right sides, extending the entire length of the spinal cord, while the are located in front of the spinal cord adjacent three large blood vessels that exit the anterior of the abdominal aorta. The prevertebral ganglia are named for the blood vessels that they are located next to; the celiac, superior mesenteric, and inferior mesenteric ganglia. The postganglionic neurons, with their cell bodies located in the prevertebral and paravertebral ganglia, extend to the target organs and are relatively long.

Figure 16.10: Connections of Sympathetic Division of the Autonomic Nervous System. (OpenStax)
The axons of the preganglionic neurons are myelinated and enter the via the . These preganglionic neurons are extensively branched and can ascend or descend targeting ganglia at multiple levels of the chain helping to generate a divergent response. The axons of the postganglionic neurons are unmyelinated and leave the sympathetic chain ganglia via the . The targets of the sympathetic nervous system are widespread and include most blood vessels. To access all these targets, including sweat glands, erector pili muscles, and cutaneous blood vessels of the skin, sympathetic postganglionic neurons travel extensively via the spinal nerves, which travel throughout the body. The preganglionic neurons that target the prevertebral ganglia travel via the splanchnic nerves (see image). Targets of these ganglia include most of the viscera (organs) and blood vessels located in the peritoneal, pleural, and pericardial cavities. The three large cervical ganglia at the top of the sympathetic chain control the head and neck’s glands and muscles (including blood vessels).

Figure 16.11: Sympathetic Connections and Chain Ganglia. (OpenStax)
Not all s terminate in a ganglion. Some innervate the of the adrenal medulla. These modified postganglionic neurons do not have dendrites or axons. Instead, they function as endocrine cells releasing hormones into the blood. These hormones are around 85% adrenalin (epinephrine) and 15% noradrenaline (norepinephrine).
The Parasympathetic Division
The parasympathetic division of the autonomic nervous system is sometimes referred to as the craniosacral division of the autonomic nervous system because all preganglionic neurons are located in the cranial nerve nuclei, the sacral spinal segments of the spinal cord (see image ). Unlike the sympathetic division, parasympathetic preganglionic neurons are very long, projecting to terminal ganglia located in the target organs. Since they arise from neurons already situated in the target organ, the postganglionic neurons are very short. Although there is some divergence in the parasympathetic division, it is not nearly as extensive as the sympathetic division.

Figure 16.12: Connections of Parasympathetic Division of the Autonomic Nervous System. (OpenStax)
The parasympathetic neurons in the cranial region travel in four of the cranial nerves: the oculomotor nerve (III), the facial nerve (VII), the glossopharyngeal nerve (IX), and the vagus nerve (X). The vagus nerve is especially important and carries almost 90% of all parasympathetic preganglionic fibers. The targets of the oculomotor nerve are controlled by the behind the eye and include constrictor muscles of the iris and the ciliary muscle that controls lens accommodation. The facial nerve controls the lacrimal glands, the submandibular and sublingual salivary glands, and the mucous membranes of the nasal cavity. The glossopharyngeal nerve controls the parotid salivary gland and the mucous membranes of the oral cavity. Finally, the vagus nerve “wanders” throughout the thoracic and abdominopelvic cavity viscera. It innervates the esophagus, heart, and lungs while the two large vagal trunks pass through the diaphragm to control the stomach, liver, pancreas, small intestine, kidney, ureter, and proximal half of the colon.
The parasympathetic fibers originating from the S2, S3, and S4 sacral spinal segments innervate much less than the cranial fibers. Targets include the distal half of the colon, the rectum, the urinary bladder, and the reproductive organs.
The Enteric Nervous System
Although it is not a part of the autonomic nervous system, the enteric nervous system also controls smooth muscle and glands of the alimentary canal. Consisting of around 100 million neurons, it is embedded in the digestive tract walls and controls gastrointestinal motility (movement) and secretion of digestive enzymes and acid. The enteric nervous system is completely functional, but its activities are modulated by the sympathetic and parasympathetic nervous systems. For example, during fight-or-flight, activity and blood flow are shifted from digestion to skeletal and cardiac muscles. The enteric nervous system is more strongly influenced by the parasympathetic division of the autonomic nervous system, and digestion occurs primarily when we are at rest. The enteric nervous system will be discussed more in the chapter on digestion.
16.3 Neurotransmitters and Receptors of the Autonomic Nervous System
![]() 16.3 Learning Outcomes
16.3 Learning Outcomes
- Know how preganglionic neurons use acetylcholine and how nicotinic acetylcholine receptors function to activate postganglionic neurons
- Understand how adrenergic receptors control the response of target organs to sympathetic stimulation
- Understand how muscarinic receptors control the response of target organs to parasympathetic stimulation
- Understand how neurotransmitter release occurs from axonal varicosities
- Know how signal cessation occurs in both the sympathetic and parasympathetic nervous systems
Preganglionic Neurons
The effects of sympathetic and parasympathetic innervation are determined by the neurotransmitters released by the postganglionic neurons and the receptors to which those neurotransmitters bind. However, before they can have their effects, they must be activated by preganglionic neurons. Preganglionic neurons for both sympathetic and parasympathetic divisions are similar in that they both release acetylcholine which binds to nicotinic acetylcholine receptors on the postganglionic neurons. Nicotinic acetylcholine receptors are the same receptors found at the neuromuscular junction. They are ionotropic receptors. This means that the receptors are ligand-gated channels. When acetylcholine (the ligand) binds to the receptor, a gate opens, allowing sodium to enter the neuron, causing the neuron to become more positive and depolarize. Therefore, when activated, the release of acetylcholine by preganglionic neurons always results in excitation of the postganglionic neuron.
Sympathetic Postganglionic Neurons
Postganglionic neurons of the sympathetic nervous system primarily use the neurotransmitter norepinephrine but occasionally use acetylcholine. The effects of norepinephrine vary depending on the type of receptor expressed by the target cell. There are two classes of receptors to which norepinephrine binds. Alpha-adrenergic and s are both metabotropic receptors and therefore work through stimulation or inhibition of second messengers, including calcium and cyclic AMP (cAMP). There are two subclasses of s, including α1 and α2. There are three classes of beta-adrenergic receptors, including β1, β2, and β3. Beta 3 receptors are less common and are found in adipose tissue but primarily in brown fat and are involved in thermogenesis. Alpha 1 and Beta 1 receptors are excitatory and work by increasing calcium (Alpha 1) or cAMP (Beta 1). Alpha 2 and Beta 2 receptors are both inhibitory and work by decreasing cAMP. As stated earlier, most postganglionic sympathetic fibers release the neurotransmitter norepinephrine. However, when stimulating sweat glands, sympathetic postganglionic neurons use acetylcholine (ACh). ACh binds to muscarinic acetylcholine receptors expressed by cells of sweat glands. This stimulates sweat glands to produce sweat. s are discussed in the next section.
Parasympathetic Postganglionic Neurons
Postganglionic neurons of the parasympathetic nervous system use acetylcholine. However, unlike the target cells of the preganglionic neurons, which express nicotinic acetylcholine receptors, targets of postganglionic neurons express muscarinic acetylcholine receptors. Like the adrenergic receptors expressed by target cells of the sympathetic nervous system, muscarinic acetylcholine receptors are metabotropic. Several subclasses of muscarinic receptors work by affecting a variety of second messenger systems. In similar ways to the adrenergic system, acetylcholine can have excitatory or inhibitory effects depending on which subclass of a receptor is expressed by the target cell.
Neurotransmitter Release
Neurotransmitter release from postganglionic neurons works differently than release from other neurons. Usually, neurons maintain a very precise and close connection with their target cells separated by only a very short distance of the synaptic cleft resulting in a 1:1 relationship between presynaptic neuron and postsynaptic neuron. Postganglionic neurons do not maintain such a precise relationship with a single neuron, nor do they have a single synaptic end bulb. Rather, postganglionic neurons have a chain of swellings or varicosities along their axons, each filled with synaptic vesicles. When stimulated by an action potential, each will release numerous vesicles of the neurotransmitter, which are showered over a broad area resulting in widespread stimulation of target cells.

Figure 16.13: Release of a Neurotransmitter from Autonomic Varicosities
Signal Cessation
After a neurotransmitter has been released and a receptor stimulated, the signal must be stopped. Acetylcholine is broken down quickly by acetylcholinesterase. Because postganglionic parasympathetic neurons release acetylcholine, the effect of parasympathetic tone is accordingly short-lived. Cessation of sympathetic signals takes longer. Norepinephrine may be transported back into the postganglionic neuron by reuptake pumps. The enzyme monoamine oxidase (MAO) can then be broken down. Any norepinephrine that diffuses away from the postganglionic neuron can be broken down by another enzyme called catechol-O-methyltransferase (COMT). Norepinephrine that COMT does not break down eventually diffuses into the blood and makes its way to the liver, where it is degraded. In general, sympathetic effects tend to last longer than parasympathetic effects because the removal of neurotransmitters and hormones released from the adrenal gland takes longer.
16.4 Autonomic Reflexes
![]() 16.4 Learning Outcomes
16.4 Learning Outcomes
- Differentiate between somatic and autonomic reflex arcs
- Compare short and long reflexes
- Describe reflex pathways
- Explain referred pain
Somatic versus Autonomic Reflexes
It is easy to imagine a somatic reflex. You start to take a spoonful of the ‘ono broth in your pho but it is way too hot. Your head jerks back quickly so you don’t burn your lips. The movement happens before your mind registers the heat. It is unconscious. But can you imagine an autonomic reflex? At the beginning of the chapter, we described a scenario with a car swerving into your lane while you are riding your scooter, thus activating your fight or flight (sympathetic) system. Your blood pressure would rapidly increase, providing more blood flow to your heart, muscles, and brain so you can quickly respond. The sight of the car swerving into your lane triggers an increase in blood pressure. That is an autonomic reflex, also called a .
In the somatic nervous system chapter, you learned about reflexes and their basic circuit–a . The information flow of a reflex arc is the sensory information coming in through a sensory afferent neuron to an integrating center located in the central nervous system and out via a motor efferent neuron to an effector. Autonomic reflexes also rely on a reflex arc, but the effectors are made of different tissues than in the somatic reflex arc. Recall that the effectors are made of skeletal muscle in the somatic nervous system, and in the ANS, the effectors are made of cardiac muscle, smooth muscle, or glands. Most of the autonomic reflex integrating centers are interneurons located in the hypothalamus, brainstem, and spinal cord that connect to preganglionic neurons. Those pathways, making connections in the CNS, are called es. However, for some autonomic reflexes–es–the signal travels from the sensory receptor cell to the peripheral ganglion to synapse with the postganglionic neuron that travels to the effector. Therefore, the short reflex pathway does not pass through the CNS.

Figure 16.14: Short and Long Reflexes. Sensory input can stimulate either a short or a long reflex. A sensory neuron can project to the CNS or an autonomic ganglion. The short reflex involves the sensory neuron’s direct stimulation of a , whereas the long reflex involves integration in the spinal cord or brain. (OpenStax)
Reflex pathways
In an autonomic (visceral) reflex, the initial input that triggers the reflex travels along the from sensory receptors toward the central nervous system. In addition to relying on sensory information from somatic and special sense receptors, the ANS also needs information about pressure and chemicals in internal organs, muscles, and the nervous system to maintain homeostasis. These sensations are detected via interoceptors for factors such as stretch in a blood vessel or pH in a body fluid. A is an example of an interoceptor. For example, baroreceptors detect blood pressure in locations such as the walls of the aorta and carotid sinuses.
Though visceral senses are not primarily a part of conscious perception, you may occasionally feel and be aware of those sensations if a visceral stimulus is strong enough. The sensory homunculus—the representation of the body in the primary somatosensory cortex—only has a small region allotted for the perception of internal stimuli. For instance, if you swallow a huge bolus of food larger than you normally swallow, you will probably feel the lump of food as it pushes through your esophagus. Sensations felt in your abdomen when your stomach is distended after eating a large meal are another example of these visceral senses. If you inhale very cold air from a refrigerator or while standing on a tall mountain such as Haleakalā or Mauna Kea, you can feel the air as it enters your larynx and trachea, thanks to these senses.
After afferent nerve fibers from visceral sensory receptors transmit signals to integrating centers, the integrating center sends signals that travel out of the central nervous system (CNS) along the of the autonomic reflex arc. This efferent pathway consists of a series of two motor neurons. The first is the preganglionic neuron that originates in the CNS and terminates in an autonomic ganglion. The second is the postganglionic neuron (also, just “ganglionic neuron”) that travels from the autonomic ganglion to the effector tissue or organ. The path of a typical visceral reflex contrasts with the somatic reflex pathway, as somatic reflexes instead only have a single motor neuron that travels from the CNS to the effector.

Figure 16.15: Comparison of Somatic and Visceral Reflexes. The afferent inputs to somatic and visceral reflexes are essentially the same, whereas the efferent branches are different. Somatic reflexes, for instance, involve a direct connection from the ventral horn of the spinal cord to the skeletal muscle. Visceral reflexes involve a projection from the to a ganglion, followed by a second projection from the ganglion to the target effector. (OpenStax)
Referred Pain
When particularly strong visceral sensations rise to the level of conscious perception, the sensations are often felt in unexpected places. For example, strong visceral sensations of the heart will likely be felt as pain in the left shoulder and left arm. This pattern of visceral sensations in one part of the body being felt as pain or sensations in a different part of the body is called . Different organ systems project their referred pain signals to different areas of the body.

Figure 16.16: Referred Pain Chart. Conscious perception of visceral sensations map to specific regions of the body, as shown in this chart. Some sensations are felt locally, whereas others are perceived as affecting areas that are quite distant from the involved organ. (OpenStax)
The location of referred pain is not random, but scientists are still working on a definitive explanation of the mechanism. The most broadly accepted theory for this phenomenon is that the visceral sensory fibers enter the same level of the spinal cord as the somatosensory fibers of the referred pain location. If we apply this theory to referred pain caused by the heart, visceral sensory fibers from the heart and surrounding mediastinal region would enter the spinal cord at the same level (middle to lower cervical) as the spinal nerves from the shoulder and arm. According to this theory, the brain misinterprets the sensations from the mediastinal region as being from the axillary and brachial regions. Another way to think of referred pain is that the signals get “crossed” between the nerves that carry signals from the heart and the nerves that carry sensations from the shoulder and arm.
16.5 Balance between sympathetic and parasympathetic activation
![]() 16.5 Learning Outcomes
16.5 Learning Outcomes
- Describe dual innervation and autonomic tone
- Differentiate between sympathetic and parasympathetic activation
Dual innervation
The autonomic nervous system is important for homeostasis because its two divisions compete at the target effector. The balance of homeostasis is attributable to the competing inputs from the sympathetic and parasympathetic divisions (dual innervation). At the cellular level, both divisions use chemical signals to activate target effector cells. A signaling molecule binds to a receptor that causes changes in the target cell, which in turn causes the tissue or organ to respond to the changing conditions of the body.
The postganglionic fibers of the sympathetic and parasympathetic divisions both release neurotransmitters that bind to receptors on their targets. Postganglionic sympathetic fibers release norepinephrine, with a few exceptions, whereas postganglionic parasympathetic fibers release acetylcholine (ACh). For any given target, the difference in which division of the autonomic nervous system is exerting control is simply determined by which neurotransmitter is binding to its receptors. The target cells will have separate adrenergic and muscarinic receptors. If norepinephrine is released, it will bind to the adrenergic receptors present on the target cell, and if ACh is released, it will bind to the muscarinic receptors on the target cell.
For most target organs and tissues of the autonomic system, their response is based on which neurotransmitter is released and what receptor is present. Dual innervation usually results in opposing ic effects between the two autonomic divisions. This antagonism is important in maintaining a set point in homeostasis. For example, regions of the heart that control how fast the heart is beating (heart rate) are innervated by postganglionic fibers from both systems. If norepinephrine is released onto those cells, it binds to adrenergic receptors that trigger certain cells of the heart to increase the rate of their action potentials, causing the heart to contract and beat faster, thus increasing your heart rate. If ACh is released onto those cells instead, it binds to a separate muscarinic receptor that causes the cells to hyperpolarize so that they take longer to reach the threshold needed to fire action potentials. This results in more time between contractions of the heart, leading to a slowing of your heart rate. Without this parasympathetic input, the heart would beat at a rate of approximately 100 beats per minute (bpm). The sympathetic system speeds that up, as it would during exercise, to 120–140 bpm, for example. The parasympathetic system slows it down to the resting heart rate of 60–80 bpm.
Another example of dual innervation is the control of pupillary size.

Figure 16.17: Autonomic Control of Pupillary Size. Activation of the pupillary reflex comes from the amount of light activating the retinal ganglion cells, as sent along the optic nerve. The output of the sympathetic system projects through the , whereas the parasympathetic system originates out of the midbrain and projects through the oculomotor nerve to the ciliary ganglion, which then projects to the iris. The postganglionic fibers of either division release neurotransmitters into the smooth muscles of the iris to cause changes in the pupillary size. Norepinephrine results in dilation, and ACh results in constriction. (OpenStax)
The afferent branch responds to light hitting the retina. Photoreceptors are activated, and the signal is transferred to the retinal ganglion cells that send an action potential along the optic nerve into the diencephalon. If light levels are low, the sympathetic system sends a signal out through the upper thoracic spinal cord to the superior cervical ganglion of the sympathetic chain. The postganglionic fiber then projects to the iris, where it releases norepinephrine onto the smooth muscle radial fibers (also pupillary dilator muscle) of the iris. When those fibers contract, the pupil dilates—increasing the amount of light hitting the retina. If light levels are too high, the parasympathetic system sends a signal out from the accessory oculomotor nucleus () through the oculomotor nerve. This fiber synapses in the ciliary ganglion in the posterior orbit. The postganglionic fiber then projects to the iris, releasing ACh onto the smooth muscle circular fibers (also, pupillary sphincter) of the iris. When circular fibers contract, the pupil constricts to limit the amount of light hitting the retina.
In this example, the autonomic system adjusts the contraction of radial fibers and circular fibers to control the pupil’s diameter, which controls how much light hits the retina. The dual innervation of the pupil is key to the reflex mechanisms that keep the activation of photoreceptors within certain limits and maintains homeostasis in sensing light.
To apply this back to the example of your threatening close encounter with a car while riding your scooter, the sympathetic response for fight or flight will increase pupillary diameter so more light hits the retina and more visual information is available for running away. Likewise, the parasympathetic response of rest reduces the amount of light reaching the retina, allowing the photoreceptors to regenerate for further visual perception by cycling through photobleaching.
There are some exceptions to competition in dual innervation. Instead of dual innervation resulting in competing or antagonistic effects, the two branches work together cooperatively in specific organs. For example, in reproduction, both branches work together. The parasympathetic nervous system is responsible for initiating and maintaining an erection in the penis, whereas the sympathetic nervous system controls reflexes that result in ejaculation. In this example, both divisions of the autonomic nervous system need to work together to accomplish a goal. Reproduction does not work without this cooperative effect.
Although many internal organs are dually innervated, there are exceptions and not all organs have dual innervation. For example, blood vessels and skin structures (for example, sweat glands and arrector pili) are innervated by only the sympathetic division. In addition, most cardiac muscle, except for the pacemaker regions, is only innervated by the sympathetic division. Therefore, only the sympathetic division controls how hard the heart is contracting. Even though some organs are only innervated by one branch, it is still possible to maintain homeostasis due to the concept of . For example, the smooth muscle found in blood vessels is always partially constricted, a state called vasomotor tone. Sympathetic fibers can increase this tone or decrease it by adjusting the rate of action potentials sent to the smooth muscle lining blood vessels. Therefore, homeostasis of the flow and pressure through blood vessels can be maintained because the blood vessels can constrict even more (vasoconstriction) or constrict less than the baseline level (vasodilation).
![]() Retrieval Practice: Pupillary Reflexes
Retrieval Practice: Pupillary Reflexes
Watch this video to learn about the pupillary reflexes. The pupillary light reflex involves sensory input through the optic nerve and motor response through the oculomotor nerve to the ciliary ganglion, which projects to the circular fibers of the iris. As shown in this short animation, pupils will constrict to limit the amount of light falling on the retina. What constitutes the afferent and efferent branches of the competing reflex (dilation)?
Autonomic Tone
Healthy organ systems can maintain a balance between sympathetic and parasympathetic activity. That balance is called autonomic tone. When something upsets the balance, homeostatic mechanisms strive to return the functions of organ systems and the body to their regular state. For each organ system, either the sympathetic or parasympathetic system may be more dominant in the resting state. Going back to the heart rate example in the previous section, the heart is an example of how one division may be dominant during rest. Because the resting heart rate is the result of the parasympathetic system slowing the heart down from its intrinsic rate of 100 bpm, the heart can be said to be in a parasympathetic tone because the parasympathetic activity is dominant and sets the current resting heart rate.
An example of sympathetic tone can also be found in a different part of the cardiovascular system. Blood pressure is partially determined by the contraction of smooth muscle in the walls of blood vessels. The smooth muscle has adrenergic receptors that are stimulated by the release of norepinephrine from postganglionic sympathetic fibers, and the smooth muscle responds by constricting and increasing blood pressure. The hormones released from the adrenal medulla—epinephrine and norepinephrine—will also bind to these receptors. Those hormones travel through the bloodstream, where they can easily interact with adrenergic receptors in the vessel walls. The parasympathetic system has no significant input from the systemic blood vessels, so the sympathetic system is solely dominant in its tone.
There are a limited number of blood vessels that respond to sympathetic input differently, and instead of constricting in response to sympathetic activity, they increase blood flow to the tissues that they supply. Examples of these exceptions include blood vessels in skeletal muscle and cardiac muscle, which are more likely to dilate in response to sympathetic activity because they have inhibitory adrenergic receptors. The dilation in these blood vessels does not have an overall effect on blood pressure nor alter the tone of these vessels, but rather allows for increased blood flow to skeletal muscles and cardiac muscles that increase their demand for oxygen and blood during the . There are a few blood vessels controlled by parasympathetic nerve fibers, but those are limited to blood vessels that supply erectile tissue of the reproductive organs. Acetylcholine released by these postganglionic parasympathetic fibers causes the vessels to dilate, leading to the engorgement of the erectile tissue.
![]() Clinical Application
Clinical Application
Orthostatic Hypotension
Have you ever stood up quickly and felt dizzy for a moment? This is because, for one reason or another, blood is not getting to your brain, briefly depriving it of oxygen. When you change position from sitting or lying down to standing, your cardiovascular system must adjust for a new challenge, keeping blood pumping up into the head while gravity is pulling more and more blood down into the legs.
The reason for this is a sympathetic reflex that maintains the output of the heart in response to postural change. When a person stands up, proprioceptors indicate that the body is changing position. A signal goes to the CNS, which then sends a signal to the upper thoracic spinal cord neurons of the sympathetic division. The sympathetic system then causes the heart to beat faster and the blood vessels to constrict. Both changes will make it possible for the cardiovascular system to maintain the rate of blood delivery to the brain. Blood is being pumped superiorly through the internal branch of the carotid arteries into the brain against the force of gravity. Gravity is not increasing while standing, but blood is more likely to flow down into the legs as they are extended for standing. This sympathetic reflex keeps the brain well oxygenated so that cognitive and other neural processes are not interrupted.
Sometimes this system does not work properly. If the sympathetic system cannot increase cardiac output, then blood pressure into the brain will decrease, and a brief neurological loss can be felt. This can be brief, such as a slight “wooziness” when standing up too quickly, or a loss of balance and neurological impairment for some time. The name for this is orthostatic hypotension, which means that blood pressure goes below the homeostatic set point when standing. It can be the result of standing up faster than the reflex can occur, which may be referred to as a benign “head rush,” or it may be the result of an underlying cause.
There are two basic reasons that orthostatic hypotension can occur. First, blood volume is too low, and the sympathetic reflex is ineffective. This hypovolemia may be the result of dehydration or medications that affect fluid balance, such as diuretics or vasodilators. Both medications are meant to lower blood pressure, which may be necessary in the case of systemic hypertension, and regulation of the medications may alleviate the problem. Sometimes, increasing fluid intake or water retention through salt intake can improve the situation.
The second underlying cause of orthostatic hypotension is autonomic failure. Several disorders result in compromised sympathetic functions. The disorders range from diabetes to multiple system atrophy (a loss of control over many systems in the body) and addressing the underlying condition can improve hypotension. For example, with diabetes, peripheral nerve damage can occur, which would affect the postganglionic sympathetic fibers. Getting blood glucose levels under control can improve neurological deficits associated with diabetes.
Sympathetic Activation
If you are making your way up Koko Head, you want to push as many nutrients and oxygen as possible to your skeletal muscles and brain.

Figure 16.18: Koko Head hike
Thankfully, physical exertion activates the sympathetic nervous system, setting you up for success to reach the summit. Sympathetic pathways are also activated by emotional stress and situations that trigger anger, anxiety, fear, and embarrassment. These feelings that lead to an emotion-driven sympathetic response may be uncomfortable, but they can be managed. If you develop a habit of mentally reframing these sympathetic responses to see the sympathetic activation as a useful mechanism to increase your success in challenging situations, it can help reduce your mind and body’s harmful responses to stress and gain a benefit from those fights or flight sensations, rather than wishing they would go away. For example, let’s imagine you are feeling nervous as you step onto the stage with your hula hui. You can consider the stress in that situation as your ally because that excitement-driven sympathetic activity gives you that increase in blood flow to your skeletal muscles and brain, making you more likely to have the strength to get through your routine and providing you with the mental recall to get each sequence as you planned. A mnemonic for recalling sympathetic responses is to think of “E” situations such as exercise, embarrassment, emergency, and excitement. See the below table for responses to sympathetic activation. Consider how each item supports the body during physical and mental exertion.
| Organ | Sympathetic | Parasympathetic |
| Heart: | Increase in heart rate and force of contraction | Decrease in heart rate |
| Blood vessels to skeletal muscles, cardiac muscle, adipose tissue, and liver: | Dilation | |
| Blood vessels to kidneys and digestive tract: | Constriction | Dilation |
| Respiration: | Dilation of airways | Constriction of airways |
| Urine formation: | Decreases | Increases |
| Digestion: | Decreases | Increases |
| Liver: | Break glycogen into glucose, increasing blood glucose | Store glucose and glycogen |
| Adipose tissue: | Break triglycerides into fatty acids and glycerol | Convert fatty acids and glycerol into triglycerides |
| Pupils: | Dilation | Constriction |
| Arrector muscles of the hair: | Contraction | |
| Sweat glands: | Secretion of perspiration | |
| Salivary glands: | Reduction of saliva | Production of saliva |
| Digestive glands and pancreas: | Release of digestive enzymes |
Table 16.2: Sympathetic and parasympathetic effects
![]() Deep Dive
Deep Dive
Have you ever watched a scary movie and during a terrifying scene the hair on your arms starts to stand up? This is called piloerection (chicken skin). Why do you suppose this happens? Have you observed this in other animals and if so, what situation were they in when their hair stood up?

Figure 16.19 (a) – above – 1) Epidermis 2) Arrector Pili muscle 3) Hair follicle 4) Dermis The diagram shows that the arrector pili muscle is connected to the hair follicle and the epidermis resulting in the erection of the hair during muscle contraction causing goosebumps. (b) – below – cat with chicken skin, human with chicken skin
 |
 |
Parasympathetic Activation
You made it onto the stage for your morning hula event, and now it’s time to enjoy a loco moco for your late breakfast.

Figure 16.20: Loco moco
The sympathetic activation from the physical exertion and excitement now needs to be toned down so you can shift into mode and relax into a parasympathetic dominant state. As discussed at the beginning of the chapter, take a few deep abdominal breaths. The feedback to your nervous system will shift from sympathetic to parasympathetic activation, setting you up for digestion of your meal and a well-deserved nap. The acronym for parasympathetic responses is SLUDD: salivation (S), lacrimation (L), urination (U), digestion (D), and defecation (D), along with three “decreases”: decreased heart rate, reduced airway diameter, and decreased pupil diameter. See the table below for parasympathetic activation responses and imagine how each supports the body during resting and digestion. Also, contrast these with the sympathetic responses.
![]() Retrieval Practice
Retrieval Practice
Sympathetic versus Parasympathetic Activation
If you used this textbook for the first half of A&P then you are by now familiar with retrieval practices. Just in case, we’ll provide a quick reminder of the process. The retrieval practice is a neuroscience-based study strategy shown to help with understanding and remembering content. The idea is to allow your retrieval practice results to inform changes you need to make in your approach to studying. Let’s start by reviewing sympathetic and parasympathetic activation. After putting away the book and your notes, start with a blank paper or clean document on your computer. List all the sympathetic and parasympathetic activations that come to mind, for example for the heart, sympathetic activations speed up heart rate and parasympathetic activation slows it down. Rather than memorizing the different activations, try to make sense of each one in the context of the setting. For example, understand why it is helpful to increase heart rate in a fight-or-flight situation and to slow it down for rest-and-digest. Do this for each organ/system you list. This way you will not be memorizing the list of activations but rather developing a sense of why your body benefits from switching between these two states in each organ/system. After you feel you can think of no other items for your list, use the book to check and correct your work. If you missed something, take a moment to create a way to remember that item in case you need to know that information for something important, like your A&P exam!
16.6 Central Control of the Autonomic Nervous System
![]() 16.6 Learning Outcomes
16.6 Learning Outcomes
- Explain how the hypothalamus integrates information and uses that information to regulate autonomic tone through control of preganglionic neurons in the brainstem and spinal cord.
- Describe the autonomic outputs of the hypothalamus
- Explain how limbic structures influence autonomic tone through inputs to the hypothalamus
- Describe the autonomic control centers of the medulla
Forebrain Structures
Autonomic control is based on the visceral reflexes, composed of the afferent and efferent branches. These homeostatic mechanisms are based on the balance between the two divisions of the autonomic system, and the function of various organs is based on whether input from the sympathetic or parasympathetic system dominates. The hypothalamus integrates various inputs and coordinates the balance that controls sympathetic and parasympathetic activity. The hypothalamus can shift our bodies between an overall sympathetic or parasympathetic tone depending on the circumstances.
The Hypothalamus
The hypothalamus is the control center for many homeostatic mechanisms. It receives input from most forebrain regions, and it regulates both autonomic function and endocrine function. In addition, the hypothalamus receives input from other areas of the forebrain through the . The olfactory cortex, the septal nuclei of the basal forebrain, and the amygdala all project into the hypothalamus through the medial forebrain bundle. These forebrain structures inform the hypothalamus about the state of the nervous system so it can adjust to the activity of organs of the body to maintain homeostasis. The amygdala is a good example of one of the structures that influence hypothalamic activity. The amygdala is found beneath the cerebral cortex of the temporal lobe and plays a role in our ability to remember and feel emotions.
Autonomic output from the hypothalamus follows two main tracts, the and the medial forebrain bundle. Along these two tracts, the hypothalamus can stimulate the accessory oculomotor nucleus (Edinger–Westphal nucleus) of the oculomotor complex, the nuclei of the vagus nerve, and the cardiac centers of the medulla, or the lateral horns of the thoracic spinal cord. These two tracts connect the hypothalamus with the major parasympathetic nuclei in the brainstem and the preganglionic neurons of the thoracolumbar and sacral spinal cord.

Figure 16.21: Fiber Tracts of the Central Autonomic System. (OpenStax)
The Amygdala
An amygdala is a group of nuclei in the medial region of the temporal lobe that is part of the (See figure ). The limbic lobe includes structures that are involved in emotions and memory. The limbic lobe has strong connections with the hypothalamus and can influence hypothalamic activity based on emotional states. For example, when you are anxious or scared, the amygdala sends signals to the hypothalamus along with the medial forebrain bundle that will stimulate the sympathetic fight-or-flight response. The amygdala will also stimulate the hypothalamus to send signals that control the endocrine system and lead to the release of stress hormones.

Figure 16.22: The Limbic Lobe. (Openstax)
The Medulla
The medulla contains nuclei, referred to as the , which controls the smooth and cardiac muscles of the cardiovascular system through autonomic connections. When changes occur in the state of your cardiovascular system, such as when blood pressure changes, the cardiovascular center can use the autonomic system to change the functioning of cardiovascular organs and tissues to bring your blood pressure back to normal. For example, anxiety and stress can stimulate the hypothalamus, which can stimulate the cardiovascular center, in turn, thus causing increased sympathetic activity in the cardiovascular system leading to a faster heart rate and increased blood pressure. The preganglionic sympathetic fibers that are responsible for increasing heart rate are referred to as the , whereas the preganglionic sympathetic fibers responsible for constricting blood vessels compose the .
Several brainstem nuclei are important for the visceral control of major organ systems. The solitary nucleus is a brainstem nucleus involved in cardiovascular function. It receives sensory input about blood pressure and cardiac function from the glossopharyngeal and vagus nerves, and output from the solitary nucleus will activate sympathetic stimulation of the heart or blood vessels through the upper thoracic lateral horn. The dorsal motor nucleus is another brainstem nucleus important for visceral control of the parasympathetic functions ascribed to the vagus nerve. The dorsal motor nucleus has many effects, including decreasing heart rate, relaxing bronchial tubes in the lungs, and activating digestive function through the enteric nervous system. The , which is named for its ambiguous histology, also contributes to the parasympathetic output of the vagus nerve and targets muscles in the pharynx and larynx involved in swallowing and speech. The nucleus ambiguous also contributes to the parasympathetic tone of the heart and the vagus dorsal motor nucleus.
16.7 Drugs and the Autonomic Nervous System
![]() 16.7 Learning Outcomes
16.7 Learning Outcomes
- Understand the difference between receptor agonists and antagonists
- Understand that, pharmaceutically, there are many ways to generate the same or very similar responses
- Know the examples of sympathomimetic and sympatholytic drugs
- Know the examples of parasympathomimetic and parasympatholytic drugs
- Understand how the autonomic nervous system relates to drug abuse
Sympathetic Effects
There are many different classes of drugs that can affect the sympathetic nervous system. In general, drugs that bind to and activate a receptor are referred to as s, whereas those that bind to and block a receptor are referred to as antagonists. Receptors that bind norepinephrine and epinephrine are referred to as adrenergic. Agonists of adrenergic receptors are sometimes referred to as sympathomimetics because they stimulate a sympathetic response. Similarly, antagonists of adrenergic receptors are sometimes referred to as sympatholytics because they inhibit or block a sympathetic response. There are many types of pharmaceutics that work this way. Although the following discussion will focus on agonists and antagonists, you should be aware that there are many other ways to get sympathomimetic and sympatholytic responses. For example, you could get a sympathomimetic response by taking drugs that bind to and activate a norepinephrine receptor (an agonist), or you could get a similar response by taking drugs that block reuptake pumps or that block monoamine oxidase or that stimulate neurotransmitter release or that stimulate/inhibit G proteins or that stimulate/inhibit enzymes that break down second messengers.
One example of a sympathomimetic is albuterol. Anyone with asthma knows what a rescue inhaler is. An albuterol inhaler is used during an asthma attack to dilate the airways. Airway dilators are called bronchodilators. Bronchodilators such as albuterol work by binding to beta-2 adrenergic receptors. Since Beta-2 adrenergic receptors cause inhibition, activating the receptor will cause the smooth muscle of the airways to relax, resulting in bronchodilation, which improves airflow. There are many other examples of s that bind to all the different types of adrenergic receptors.
On the other hand, s work by inhibiting or blocking a sympathetic response. There are many ways this can happen, but we focus on agonists and antagonists. An excellent example of this type of medication is a class of drugs called beta-blockers. Beta-blockers, such as propranolol, bind to adrenergic beta receptors, but, unlike albuterol, they do not activate the receptors. Rather they block epinephrine and norepinephrine from binding to and activating the receptors. The primary use of this class of medication is to lower blood pressure. By blocking the sympathetic response, the heart rate and contractility will decrease, thus lowering cardiac output, which results in lower blood pressure.
Parasympathetic Effects
Just as the adrenergic receptors of the sympathetic nervous system can be stimulated or inhibited, the muscarinic receptors of the parasympathetic nervous system can likewise be stimulated or inhibited. Muscarinic agonists result in a parasympathomimetic effect, whereas muscarinic antagonists generate a parasympatholytic effect. As with the sympathetic nervous system, there are many ways to stimulate or inhibit the system.
One example of a is methacholine. It can help diagnose asthma by triggering bronchoconstriction. The methacholine challenge test helps clinicians determine sensitive or reactive airways. When inhaled, methacholine will bind and activate muscarinic acetylcholine receptors in the airways, causing them to bronchoconstrict.
As with sympatholytic drugs, many parasympatholytics function as antagonists of the muscarinic acetylcholine receptors. One example of a muscarinic antagonist that generates a parasympatholytic response is atropine. Among other things, atropine can be used to treat bradycardia which is a low heart rate. However, when atropine binds to the muscarinic receptor, it does not activate it. Rather, it prevents acetylcholine from binding to and activating the receptor, thus generating the parasympatholytic response and elevating the heart rate.
Drug Abuse
Many commonly abused drugs generate sympathetic or parasympathetic responses. For example, cocaine blocks monoamine (such as dopamine and norepinephrine) reuptake pumps. This results in more norepinephrine binding to their receptors, generating a sympathomimetic response, including elevated heart rate, blood pressure, and pupil dilation. Similarly, amphetamines work by causing more dopamine and norepinephrine release again, resulting in more norepinephrine binding to their receptors and generating a sympathomimetic response similar to cocaine. Other drugs, such as heroin and morphine, have a parasympathomimetic response by shifting autonomic tone in the brain. This results in parasympathetic responses such as bradycardia, inhibition of respiration, and pupil constriction. In the emergency room, physicians are trained to observe patients’ eyes, looking for the dilated pupils familiar with stimulant abuse or the “pinpoint pupils” common in patients abusing opiates.
![]() Food and Environment: ʻAwa for Anxiety
Food and Environment: ʻAwa for Anxiety
E hānai ‘awa a ikaika ka makani.
Feed with kava so that the spirit may gain strength
Olelo No’eau, Collected by Mary Kawena Pukui, #275
Have you ever been to a kava bar? ʻAwa (Piper methysticum), which is also known as kava, is a canoe plant (introduced to the Hawaiian Islands by Polynesians) and is a shrubby plant that belongs to the pepper family. ʻAwa grows in moist and shady areas of the lower forest zones and has grown throughout Oceania for its various medicinal effects, including a remedy for anxiety, nervousness, and insomnia. Traditionally, fresh or dried ʻawa roots were prepared into ceremonial drinks by chewing the roots to soften them, then soaking them in water. These days, the ʻawa drinks have increased in popularity. There are now kava bars that specialize in serving kava drinks, and kawa is sold as a dietary supplement as a tincture, and in capsules. Scientists are also studying the medicinal and chemical properties of ʻawa. Various studies have shown the therapeutic effects of ʻawa in patients with mild to moderate anxiety. Interestingly, some studies also show kavaʻs potential in reducing cancer risk. Now, scientists are looking into different active components of kava ingredients to understand the effects of kava even further!
https://www.mdpi.com/2072-6643/12/10/3044/htm
 |
 |
| ʻAwa plant | Prepared kava drink |
Figure 16.23: ʻAwa
![]() Cultural Connection: Lōkahi and Balance
Cultural Connection: Lōkahi and Balance
The music is in one pitch and the voice in another
Said of a lack of harmony
ʻOlelo Noʻeau, collected by Mary Kawena Pukui, #735
Native Hawaiians believe that health and wellness are achieved through a balanced interdependent relationship between uhane (spirit), kino (body/physical), and mana‘o (mind/emotions, including thoughts, beliefs, ideas, and feelings). One term used to describe this is lōkahi, which is often defined as unity or balance, and balance between an individual’s mind, body, spirit, and the whole world. One way to visualize this balance is using the Lōkahi Wheel, first introduced by Kamehameha Schools, which represents six sections of the life of a kanaka: Spiritual/Soul, Friends/Family, Physical/Body, Work/School, Thinking/Mind, and Feelings/Emotions. An imbalance in the anchors of the lōkahi wheel is thought to be a cause of illness. For example, humans can get into a disordered physical state if the friends/family aspect of their life is disrupted. The concept of the Lōkahi Wheel predates and yet is also aligned with contemporary practices of functional medicine, in which treatment of homeostatic imbalance is not based on drug intervention but rather on determining the root cause of the imbalance itself in an effort to return to balance.
 Now that we have discussed the lōkahi wheel and balance, can you think of a connection between lomilomi and balance? How do you think lomilomi impacts the parasympathetic system?
Now that we have discussed the lōkahi wheel and balance, can you think of a connection between lomilomi and balance? How do you think lomilomi impacts the parasympathetic system?
![]() Local Issue
Local Issue
Hawaiʻi has a higher cost of living than any U.S. state on the continent. The high cost of living in Hawaiʻi can create health problems as well. A sympathetic dominant state can result from overwork and lack of sleep. This sympathetic dominant state can lead to disease and disorders such as high blood pressure and stress. When the cost of living is taken into account, Hawaiʻi has a higher poverty rate than the U.S. average, with anywhere from 14–16% of Hawaiʻi residents living in poverty. While the official unemployment rate in Hawaiʻi is generally low, this statistic conceals the fact that many people in Hawaiʻi must work multiple jobs to pay for housing and basic necessities. The combined stress, overwork, and lack of sleep that result from these living conditions create an unhealthy situation across the board. Many of the permanent residents of Hawaiʻi are negatively impacted by these unhealthy conditions and are put at higher risk for a variety of health and social problems that result from sleep deficits, chronic stress, and overwork. One possible solution would be to ensure that official statistics more accurately convey the actual situation in Hawaiʻi so that organizations working on the issues have useful data and that public funding is not denied to Hawaiʻi residents living below the poverty line because of faulty measurements of poverty. Another initiative that may help is a renewed focus on local food production rather than a continued reliance on imported supplies.
![]() Retrieval Practice
Retrieval Practice
Study tip for structures that receive only sympathetic innervation: ABE, Adrenal Medulla, Blood Vessels, and Effectors of skin (arrector pili muscles and sweat glands. ABE: Alex Bit Elephant.

Chapter Summary

Key Terms
acetylcholine (ACh)
neurotransmitter that binds at a motor end-plate to trigger depolarization
adrenal medulla
interior portion of the adrenal (or suprarenal) gland that releases epinephrine and norepinephrine into the bloodstream as hormones
adrenergic
synapse where norepinephrine is released, which binds to α- or β-adrenergic receptors
afferent branch
component of a reflex arc that represents the input from a sensory neuron, for either a special or general sense
agonist
any exogenous substance that binds to a receptor and produces a similar effect to the endogenous ligand
alpha (α)-adrenergic receptor
one of the receptors to which epinephrine and norepinephrine bind, which comes in two subtypes: α1 and α2
antagonist
any exogenous substance that binds to a receptor and produces an opposing effect to the endogenous ligand
autonomic tone
tendency of an organ system to be governed by one division of the autonomic nervous system over the other, such as heart rate being lowered by parasympathetic input at rest
baroreceptor
mechanoreceptor that senses the stretch of blood vessels to indicate changes in blood pressure
beta (β)-adrenergic receptor
one of the receptors to which epinephrine and norepinephrine bind, which comes in three subtypes: β1, β2, and β3
cardiac accelerator nerves
preganglionic sympathetic fibers that cause the heart rate to increase when the cardiovascular center in the medulla initiates a signal
cardiovascular center
region in the medulla that controls the cardiovascular system through cardiac accelerator nerves and vasomotor nerves, which are components of the sympathetic division of the autonomic nervous system
central neuron
specifically referring to the cell body of a neuron in the autonomic system that is located in the central nervous system, specifically the lateral horn of the spinal cord or a brain stem nucleus
chromaffin cells
neuroendocrine cells of the adrenal medulla that release epinephrine and norepinephrine into the bloodstream as part of sympathetic system activity
ciliary ganglion
one of the terminal ganglia of the parasympathetic system, located in the posterior orbit, axons from which project to the iris
dorsal longitudinal fasciculus
major output pathway of the hypothalamus that descends through the gray matter of the brain stem and into the spinal cord
Edinger–Westphal nucleus
location of parasympathetic neurons that project to the ciliary ganglion
efferent branch
component of a reflex arc that represents the output, with the target being an effector, such as muscle or glandular tissue
epinephrine
signaling molecule released from the adrenal medulla into the bloodstream as part of the sympathetic response
fight-or-flight response
set of responses induced by sympathetic activity that lead to either fleeing a threat or standing up to it, which in the modern world is often associated with anxious feelings
ganglionic neuron
specifically refers to the cell body of a neuron in the autonomic system that is located in a ganglion
gray rami communicantes
(singular = ramus communicans) unmyelinated structures that provide a short connection from a sympathetic chain ganglion to the spinal nerve that contains the postganglionic sympathetic fiber
limbic lobe
structures arranged around the edges of the cerebrum that are involved in memory and emotion
long reflex
reflex arc that includes the central nervous system
medial forebrain bundle
fiber pathway that extends anteriorly into the basal forebrain, passes through the hypothalamus, and extends into the brain stem and spinal cord
muscarinic receptor
type of acetylcholine receptor protein that is characterized by also binding to muscarine and is a metabotropic receptor
norepinephrine
signaling molecule released as a neurotransmitter by most postganglionic sympathetic fibers as part of the sympathetic response, or as a hormone into the bloodstream from the adrenal medulla
nucleus ambiguus
brain-stem nucleus that contains neurons that project through the vagus nerve to terminal ganglia in the thoracic cavity; specifically associated with the heart
parasympathetic division
division of the autonomic nervous system responsible for restful and digestive functions
parasympathomimetic drugs
drugs that enhance or mimic the function of the parasympathetic system
paravertebral ganglia
autonomic ganglia superior to the sympathetic chain ganglia
postganglionic fiber
axon from a ganglionic neuron in the autonomic nervous system that projects to and synapses with the target effector; sometimes referred to as a postganglionic neuron
preganglionic fiber
axon from a central neuron in the autonomic nervous system that projects to and synapses with a ganglionic neuron; sometimes referred to as a preganglionic neuron
prevertebral ganglia
autonomic ganglia that are anterior to the vertebral column and functionally related to the sympathetic chain ganglia
referred pain
the conscious perception of visceral sensation projected to a different region of the body, such as the left shoulder and arm pain as a sign for a heart attack
reflex arc
circuit of a reflex that involves a sensory input and motor output, or an afferent branch and an efferent branch, and an integrating center to connect the two branches
rest and digest
set of functions associated with the parasympathetic system that lead to restful actions and digestion
short reflex
reflex arc that does not include any components of the central nervous system
somatic reflex
reflex involving skeletal muscle as the effector, under the control of the somatic nervous system
superior cervical ganglion
one of the paravertebral ganglia of the sympathetic system that projects to the head
sympathetic chain ganglia
series of ganglia adjacent to the vertebral column that receive input from central sympathetic neurons
sympathetic division
division of the autonomic nervous system associated with the fight-or-flight response
sympatholytic drug
drug that interrupts, or “lyses,” the function of the sympathetic system
sympathomimetic drug
drug that enhances or mimics the function of the sympathetic system
target effector
organ, tissue, or gland that will respond to the control of an autonomic or somatic or endocrine signal
terminal ganglia
ganglia of the parasympathetic division of the autonomic system, which are located near or within the target effector, the latter also known as intramural ganglia
varicosity
structure of some autonomic connections that is not a typical synaptic end bulb, but a string of swellings along the length of a fiber that makes a network of connections with the target effector
vasomotor nerves
preganglionic sympathetic fibers that cause the constriction of blood vessels in response to signals from the cardiovascular center
visceral reflex
reflex involving an internal organ as the effector, under the control of the autonomic nervous system
white rami communicantes
(singular = ramus communicans) myelinated structures that provide a short connection from a sympathetic chain ganglion to the spinal nerve that contains the preganglionic sympathetic fiber
Attribution: Some sections of this chapter have been modified from OpenStax A&P
Media Attributions
- olelo_noeau
- Autonomic and Somatic Nervous System © Christinelmiller is licensed under a CC BY-SA (Attribution ShareAlike) license
- Love is on the way © Micah Camara is licensed under a CC BY-NC-ND (Attribution NonCommercial NoDerivatives) license
- Pathways of motor neurons © Helixitta adapted by LynleyShimat Lys is licensed under a CC BY-SA (Attribution ShareAlike) license
- Autonomic Nervous System A © Macleod, John James Rickard, 1876-1935 Pearce, R. G. (Roy Gentry), 1884- is licensed under a Public Domain license
- Autonomic Nervous System: Schematic Representation © Macleod, John James Rickard, 1876-1935 Pearce, R. G. (Roy Gentry), 1884- is licensed under a Public Domain license
- Somatic Autonomic and Enteric Structures of the Nervous System © OpenStax is licensed under a CC BY (Attribution) license
- Autonomic Sympathetic Nerves © Campos-Rodríguez R, Godínez-Victoria M, Abarca-Rojano E, Pacheco-Yépez J, Reyna-Garfias H, Barbosa-Cabrera RE, Drago-Serrano ME is licensed under a CC BY (Attribution) license
- Adrenal Medulla © http://www.scientificanimations.com is licensed under a CC BY-SA (Attribution ShareAlike) license
- Connections of the Parasympathetic Division of the Autonomic Nervous System © OpenStax adapted by LynleyShimat Lys is licensed under a CC BY (Attribution) license
- OS Connections Sympathetics Division ANS
- OS Sympathetic Connections and Chain Ganglia © OpenStax is licensed under a CC BY (Attribution) license
- Release of a Neurotransmitter from Autonomic Varicosities © OpenStax is licensed under a CC BY (Attribution) license
- OS Short and Long Reflexes © OpenStax is licensed under a CC BY (Attribution) license
- Comparison of Somatic and Visceral Reflexes © OpenStax is licensed under a CC BY (Attribution) license
- Referred Pain Chart © Openstax is licensed under a CC BY (Attribution) license
- Autonomic Control of Pupillary Size © OpenStax is licensed under a CC BY (Attribution) license
- Koko Head Hike © Thomas Woodtli is licensed under a CC BY-SA (Attribution ShareAlike) license
- Piloerection (Chicken Skin) Animation © AnthonyCaccese is licensed under a CC BY-SA (Attribution ShareAlike) license
- Piloerection (Chicken Skin) Cat © SKsiddhartthan is licensed under a CC BY-SA (Attribution ShareAlike) license
- Piloerection (Chicken Skin) Goosebumps © Ildar Sagdejev (Specious) is licensed under a CC BY-SA (Attribution ShareAlike) license
- Loco Moco © christian razukas is licensed under a CC BY-SA (Attribution ShareAlike) license
- Fiber Tracts of the Central Autonomic System © OpenStax is licensed under a CC BY (Attribution) license
- The Limbic Lobe © OpenStax is licensed under a CC BY (Attribution) license
- ʻAwa plant Piper methysticum © Forest & Kim Starr is licensed under a CC BY (Attribution) license
- Prepared Kava Drink © Dave Lonsdale is licensed under a CC BY (Attribution) license
- Lōkahi Wheel © LynleyShimat Lys is licensed under a CC BY (Attribution) license
- Honu_‘Iwalani Clayton_CCBY_2022 10 30 © ‘Iwalani Clayton is licensed under a CC BY (Attribution) license
- divider_maile
division of the autonomic nervous system responsible for restful and digestive functions
reflexes with effectors consisting of skeletal muscle
neurotransmitter that binds at a motor end-plate to trigger depolarization
secondary catecholamine hormone secreted by the adrenal medulla in response to short-term stress; also called noradrenaline
primary and most potent catecholamine hormone secreted by the adrenal medulla in response to short-term stress; also called adrenaline
inner layer of the adrenal glands that plays an important role in the stress response by producing epinephrine and norepinephrine
ganglia of the parasympathetic division of the autonomic system, which are located near or within the target effector, the latter also known as intramural ganglia
specifically refers to the cell body of a neuron in the autonomic system that is located in a ganglion
organ, tissue, or gland that will respond to the control of an autonomic or somatic or endocrine signal
division of the autonomic nervous system associated with the fight-or-flight response
autonomic ganglia superior to the sympathetic chain ganglia
autonomic ganglia that are anterior to the vertebral column and functionally related to the sympathetic chain ganglia
autonomic ganglia in a chain along the anterolateral aspect of the vertebral column that are responsible for contributing to homeostatic mechanisms of the autonomic nervous system
(singular = ramus communicans) myelinated structures that provide a short connection from a sympathetic chain ganglion to the spinal nerve that contains the preganglionic sympathetic fiber
(singular = ramus communicans) unmyelinated structures that provide a short connection from a sympathetic chain ganglion to the spinal nerve that contains the postganglionic sympathetic fiber
axon from a central neuron in the autonomic nervous system that projects to and synapses with a ganglionic neuron; sometimes referred to as a preganglionic neuron
neuroendocrine cells of the adrenal medulla that release epinephrine and norepinephrine into the bloodstream as part of sympathetic system activity
one of the terminal ganglia of the parasympathetic system, located in the posterior orbit, axons from which project to the iris
synapse where norepinephrine is released, which binds to α- or β-adrenergic receptors
one of the receptors to which epinephrine and norepinephrine bind, which comes in three subtypes: β1, β2, and β3
one of the receptors to which epinephrine and norepinephrine bind, which comes in two subtypes: α1 and α2
type of acetylcholine receptor protein that is characterized by also binding to
muscarine and is a metabotropic receptor
structure of some autonomic connections that is not a typical synaptic end bulb, but a string of swellings along the length of a fiber that makes a network of connections with the target effector
reflex involving an internal organ as the effector, under the control of the autonomic nervous system
reflex pathway consisting of receptor, sensory afferent neuron, integration or reflex center, motor efferent neuron and effector
reflex arc that includes the central nervous system
reflex arc that does not include any components of the central nervous system
axon from a ganglionic neuron in the autonomic nervous system that projects to and synapses with the target effector; sometimes referred to as a postganglionic neuron
component of a reflex arc that represents the input from a sensory neuron, for either a special or general sense
mechanoreceptor that senses the stretch of blood vessels to indicate changes in blood pressure
component of a reflex arc that represents the output, with the target being an effector, such as muscle or glandular tissue
specifically referring to the cell body of a neuron in the autonomic system that is located in the central nervous system, specifically the lateral horn of the spinal cord or a brain stem nucleus
when pain is perceived at a location other than the site of the painful stimulus
muscle that opposes the action of an agonist
one of the paravertebral ganglia of the sympathetic system that projects to the head
location of parasympathetic neurons that project to the ciliary ganglion
tendency of an organ system to be governed by one division of the autonomic nervous system over the other, such as heart rate being lowered by parasympathetic input at rest
set of responses induced by sympathetic activity that lead to either fleeing a threat or standing up to it, which in the modern world is often associated with anxious feelings
set of functions associated with the parasympathetic system that lead to restful actions and digestion
fiber pathway that extends anteriorly into the basal forebrain, passes through the hypothalamus, and extends into the brain stem and spinal cord
major output pathway of the hypothalamus that descends through the gray matter of the brain stem and into the spinal cord
structures arranged around the edges of the cerebrum that are involved in memory and emotion
region in the medulla that controls the cardiovascular system through cardiac accelerator nerves and vasomotor nerves, which are components of the sympathetic division of the autonomic nervous system
preganglionic sympathetic fibers that cause the heart rate to increase when the cardiovascular center in the medulla initiates a signal
preganglionic sympathetic fibers that cause the constriction of blood vessels in response to signals from the cardiovascular center
brain-stem nucleus that contains neurons that project through the vagus nerve to terminal ganglia in the thoracic cavity; specifically associated with the heart
(also, prime mover) muscle whose contraction is responsible for producing a particular motion
drug that enhances or mimics the function of the sympathetic system
drug that interrupts, or “lyses,” the function of the sympathetic system
drugs that enhance or mimic the function of the parasympathetic system
