Anatomy and Physiology
4 Tissue
 ʻAʻohe hana nui ke alu ʻia.
ʻAʻohe hana nui ke alu ʻia.
No task is too big when done together by all
ʻŌlelo Noʻeau, compiled by Mary Kawena Pukui, #142
Introduction
Four Types of Tissue
| Connective Tissue
|
Epithelial Tissue
|
| Muscle Tissue
|
Nervous Tissue
|
Fig. 4.1: Grid of different tissues
![]() Chapter Learning Outcomes
Chapter Learning Outcomes
- Identify the 4 broad tissue types of the human body
- Understand the relationship between structure and function regarding all four tissue types
- Identify the connection between epithelial tissue and connective tissue and describe how they work together to form various membranes
- Identify the unique properties of each tissue with a focus on epithelial tissue and connective tissue
- Understand how tissues change in health and disease
4.1 Introduction to Tissues
The human body is composed of trillions of cells. This tremendous amount of cells can be condensed and categorized into roughly 200 different individual types. Further, these various types of cells don’t typically work as isolated units, instead, they work together in groups called . Just like weaving a lauhala mat from lau, the leaves of the hala tree, various cells involved with the tissue work together to carry out a similar function in the body. Depending on the combination of cells and how they were put together, the resulting tissue can carry out specific functions, just as different weaves of lau contribute to different textures and strengths of the mat. The trillions of cells working together form 4 basic tissue types: epithelial, connective, muscle, and nerve.

Fig. 4.2: Four Types of Tissue
, also referred to as epithelium, refers to the sheets of cells that cover exterior surfaces of the body, line internal cavities and passageways, and form certain glands. , as its name implies, binds the cells and organs of the body together and functions in the protection, support, and integration of all parts of the body. is excitable, responding to stimulation and contracting to provide movement. is also excitable, allowing the propagation of electrochemical signals in the form of nerve impulses that communicate between different regions of the body.
This chapter will focus primarily on epithelial and some connective tissues. Bone (a supporting connective tissue), cartilage, muscle, and nervous tissues are covered in greater detail in further chapters when appropriate.
Recall from the previous chapter the levels of organization: chemical level→ cellular level→ tissue level→ organ level→ system level→ organism level. This chapter covers the properties of various tissues.
The word kilo means to watch closely, examine, or observe. The practice of kilo refers to observing the environment around us, but the same concept can be applied when observing the environment within us. To study the human organism on the tissue level, we must use equipment such as a microscope to enhance what is seen. So, in Anatomy and Physiology, we practice kilo every day, but especially when we view structures at the tissue level. Because we are so used to seeing gross anatomy, it can oftentimes be confusing to connect a slide of the skin to the gross (epidermis of the skin) we can see and touch daily. When we kilo, we observe deeply, notice the smallest details, and use our observations to learn. For example, even though we may be looking at a slide of epithelial tissue, if we look closely, we may see connective tissue such as adipose on the same slide. Through observation, we can see the interconnectedness that exists between tissues in the human body and recognize that relative location has ties to a tissue’s function. If we observe two different tissue types next to each other, and we can tell that they are two different types of tissue, then we can begin to make connections between the two.
4.2 Epithelial Tissues
![]() 4.2 Learning Outcomes
4.2 Learning Outcomes
- Describe the various types of epithelial tissue.
- Understand their function as it relates to their form.
General Characteristics of Epithelial Tissue
Epithelial tissue is divided into two main divisions: tissue that covers and lines body surfaces and hollow spaces in the body, and glandular tissue. Epithelial tissue (unlike connective tissue) is composed of closely joined cells with minimal intercellular (between cells) material. The cells that make up epithelial tissues typically have a high mitotic (cell division) rate. It is important to note that epithelial tissues are innervated (have a nerve supply), however, it is avascular (does not have a blood supply). In other words, no blood vessels permeate throughout the cells of epithelial tissue. Living cells are constantly metabolizing and therefore require delivery of oxygen and nutrients and removal of waste products (such as carbon dioxide). For this reason, you will notice that epithelial tissue is always closely bordered by connective tissue, (a vascular tissue) and is adhered to it by way of a .
(a)
(b)

Fig 4.3: (a) Image of cell layer with basement membrane (b) Apical and Basal Surface
The basement membrane also called the consists of a layer of protein and glycoprotein (part carbohydrate, part protein) fibers that anchor epithelial tissue to the underlying connective tissue. By bordering on a vascular connective tissue the living cells making up the epithelial can get their demands met by way of diffusion of substances in and out of the cell via nearby blood vessels. As you will see in future examples of stratified (multi-layered) epithelial tissue, mitosis of newer cells at the basement membrane pushes the older cells further from the bordering connective tissue and blood supply, and as these older cells migrate further and further away from the support of the vascular connective tissue they will begin to die and slough off.
Recall that epithelial tissues are border and boundary tissues. They cover body surfaces, line body cavities, and form walls of ducts and blood vessels. Therefore, there will be a side of this tissue that faces these openings. The portion of this tissue that is exposed to the body cavity, lumen, internal organ, or exterior of the body is known as the “free” surface. The sides of the cells making up the tissue that face the border with the connective tissue are considered the basal “basement” surface.
The apical surface of epithelial tissue may be lined with microvilli or cilia. This is another great example of form following function. Epithelial cells that have microvilli on their apical surface are typically involved with some type of secretion or absorption. Microvilli are numerous tiny finger-like projections that drastically increase the surface area of the apical cell membrane and therefore that of the overall tissue. The increased surface area promotes efficient diffusion or transport and the movement of substances across the apical membrane into or out of the cell.
Certain epithelial cells contain cilia, as explained in Chapter 3. Cilia are typically mobile as they contain contractile proteins throughout their structure, allowing the cilia to beat back and forth in a rhythmic manner. The movement of cilia promotes the movement of substances along the apical surface. A great example of this ciliary movement is the respiratory epithelium that lines the trachea and bronchi. The cilia are constantly trapping and moving particulates that one breathes in. These particulates get stuck in the mucous that this tissue produces and the cilia methodically move the particulates up the bronchi and trachea to the throat where it is swallowed. This combination of mucus and cilia moving particles up the airways is sometimes referred to as the mucociliary escalator.
Many epithelial tissues are major components of s which will be discussed later in this chapter. Mucus is a slippery substance secreted by s or larger glands. Goblet cells are considered unicellular glands that are dispersed among the other cells in epithelial tissue. Most often they are found lining the gastrointestinal and respiratory tracts in simple columnar and pseudostratified epithelial tissue.
(a)

(b)

Fig 4.4: Goblet Cell (a) In the lining of the small intestine, columnar epithelium cells are interspersed with goblet cells. (b) The arrows in this micrograph point to the mucous-secreting goblet cells. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Classification of Epithelial Tissue
Many types of epithelial tissue serve as a protective layer. When epithelial tissue is used for protection, it is made up of multiple layers of cells that help to defend the body against abrasion or chemical insult. As you may have guessed, the outer layer of the skin is made up of many multiple layers of epithelial cells and serves as a protective and effective barrier to the outside world.
The naming strategy to identify the various types of epithelial tissue is quite simple. These are identified and named by the number of cell layers (strata) and cell shape (Figure 4.5).

Fig 4.5: Cells of Epithelial Tissue. Simple epithelial tissue is organized as a single layer of cells and stratified epithelial tissue is formed by several layers of cells.
Simple Epithelium
Epithelial tissue that is composed of a single layer is called simple.
Squamous: consists of a single layer of flattened epithelial cells. Due to its thin makeup, it is ideal for promoting diffusion, excretion, and absorption. It is found in portions of the body such as the alveoli (air sacs) of the lungs and capillaries. Here the epithelial tissue promotes the diffusion of both oxygen and carbon dioxide gases across the cell into and out of the blood. It is also a part of the visceral and parietal serosal membranes of the body cavities (mentioned in the introductory chapter). In this instance, the simple squamous epithelium is responsible for secreting serous fluid. If you are viewing simple squamous epithelium from a superior view [simple squamous superior view] you would see a sheet of cells that appear to look like numerous eggs tossed into a frying pan with cell borders that are all irregular in shape. If you were to view this tissue from a lateral view you would see a thin (squamous meaning flat) layer of cells bulging slightly at the location of the nucleus [lateral view simple squamous epithelium]. In other words, imagine looking at a sheet of paper from two different angles, if you looked at the sheet of paper from the top you would see a large surface area of the paper. If you looked at the side of the paper at eye level you would only see a very thin layer of the paper.

Fig. 4.6: Simple squamous epithelium
![]() Clinical Application
Clinical Application
As with most habits, smoking is a difficult one to get rid of. A lot of times, this habit starts in our teenage years and continues to our adulthood. We know that smoking and “vaping” are bad for our respiratory system. What about the effects of smoking on other body systems? Why is smoking so bad for our tissues?
In a non-smoker, the simple squamous epithelium found in the alveoli within the lungs is healthy, meaning the alveoli are small, well-formed and there are plenty of them! In a smoker, the alveoli are enlarged, have black deposits, and are far less numerous. The reduction in the number of alveoli causes a decrease in the surface area available for gas exchange, making breathing more difficult. Smoking increases the risk of getting several diseases, such as emphysema and lung cancer. In emphysema, the destruction of the walls in the alveoli not only makes breathing more difficult but also increases coughing. Lung cancer happens in the epithelium of the respiratory tract and one main problem of this disease is that cancer can travel to other parts of the body due to the presence of blood vessels and lymphatic vessels within the lungs.
So, how can smoking also affect other parts of our bodies? Nicotine causes vasoconstriction and as a result, we have a reduction in blood flow, which decreases the arrival of nutrients and removal of wastes within the systemic tissues in other parts of our bodies. The vasoconstriction can also affect the arteries of a pregnant woman, who would have fewer nutrients delivered to the placenta and as a result, her baby may be born with health issues, such as being underweight. Is vaping or smoking e-cigarettes better for our health in comparison with regular cigarettes? Not really. Both contain nicotine and other harmful substances.

Fig. 4.7: Simple cuboidal epithelium
Cuboidal: As the name suggests, the consists of a single layer of cube-shaped cells. Under a microscope, they appear to be more cuboidal than round, flat, or column-like. Simple cuboidal is also found where excretion and absorption take place. It makes up various glands, ducts, and portions of the kidney tubules.

Fig. 4.8: Simple columnar epithelium
Columnar: can be identified by their column-like or rectangular shape. It should be noted that in many instances the observer may have trouble distinguishing between cuboidal and columnar as the shapes may not always be so obvious. Usually, with columnar epithelium, the cells’ nuclei are elongated and will appear closer to the basement membrane than the apical surface. If the nuclei are round and appear to be situated approximately in the middle of the cell, it is most likely cuboidal. The columnar epithelium is found lining the luminal surface of the gastrointestinal (GI) tract starting with the stomach and continues throughout the small and large intestine. This tissue is involved with excretion and absorption. For example, a group of cells making up the simple columnar tissue in the stomach are involved with the excretion of hydrochloric acid that aids in digestion whereas further down in the small intestine, the epithelial lining is involved with the absorption of various nutrients and water. Here the simple columnar epithelium will contain numerous microvilli on the apical surface to increase surface area promoting this absorption. This is another excellent example of the form following function.
Stratified Epithelium
Epithelial tissue that is composed of more than one layer is called stratified.
Stratified Squamous

Fig. 4.9: Stratified squamous epithelium
depending on the location it may form several layers thick. This tissue is found in areas where abrasion takes place and there are mechanical or chemical stresses on the tissue. It functions as a protective barrier. Stratified squamous epithelium is found making up the surface of the skin, lining the inside of the mouth, esophagus, and anus. The cells making up stratified squamous epithelium tend to be cuboidal in shape near the basement membrane, however, as mitosis of these stem cells proceed and the older cells are pushed further and further away from the basal border with connective tissue (their blood supply), they begin to flatten and die. It may be confusing to the student as you look at a lateral view of stratified squamous epithelium under a microscope as the cells at the basal side of the tissue appear to be cuboidal, however, keep in mind that the tissue is named based on the shapes of the cells on the apical surface of the tissue.
On the body surface (skin) where possible dehydration poses a problem, the stratified squamous epithelium contains keratin. Keratin is a water-resistant protein that minimizes the amount of water loss from the body. Therefore epithelial tissue that contains keratin is considered to be keratinized stratified squamous epithelium. In moist areas inside the body where abrasion is also a potential hazard, such as the esophagus, the vagina, the anal canal, and the urethra, the tissue lacks keratin and is therefore called non-keratinized stratified squamous epithelium.

Fig. 4.10: Stratified cuboidal epithelium
Cuboidal: is not common. It is found in ducts of various sweat glands permeating through various layers of the skin and portions of mammary gland ducts.

Fig. 4.11: Stratified columnar epithelium
Columnar: is also quite rare. It is found in limited areas of the pharynx (throat), epiglottis, and ducts of the parotid salivary glands. Stratified columnar epithelium may be 2 or multiple cell layers thick. If it is multiple cell layers thick only the cells facing the apical surface are columnar.
Pseudostratified Epithelium

Fig. 4.12:
Pseudostratified: This type of tissue cannot be easily classified by cell layers. As the name pseudo implies, this columnar epithelium has the appearance of stratification because the nuclei are found at multiple levels rather than situated close to the basement membrane as seen with typical columnar cells. However, with pseudostratified columnar epithelia, all of the columnar cells are attached to the basement membrane and are therefore not truly stratified. Pseudostratified columnar epithelium typically has cilia. The pseudostratified ciliated columnar epithelium is a mouthful so it is sometimes abbreviated PCCE. This ciliated epithelium is found lining most portions of the respiratory tract (as mentioned above) and is involved with protection, secretion of mucous, and movement of substances across its apical surface.
Transitional Epithelium

Fig. 4.13: Transitional epithelium
Transitional: cannot be easily classified by cell shapes. This type of tissue can tolerate stretch and recoil in repeated cycles. When stretched the apical cells of this tissue appear to be flattened. However, with recoil, the apical cells in this tissue transition into a more cuboidal shape, often bulging out into the lumen. Transitional epithelium is found in areas of stretching such as the urinary bladder and ureters.
![]() Retrieval Practice
Retrieval Practice
Put away the book and all of your notes. Make some very rough sketches of each of the seven types of epithelial tissue. Label each type. Remember part of the skill you are developing is to make quick rough sketches, so do not spend too much time on that part. After you have sketched as many as you can recall, add arrows with words describing anything you can recall about each of the types, for example, what is a major characteristic or function of that type of epithelial tissue. Take a moment to congratulate yourself for all you were able to create, and then go back to the chapter and add in any missing details and functions on your sketches while also making corrections to any of your errors.
4.3 Intercellular Connections
![]() 4.3 Learning Outcome
4.3 Learning Outcome
- Describe the different types of intercellular connections between cells.
One of the hallmarks of epithelial tissues is that the cells are physically connected through various junctions (a place or structure of joining). s provide gaps (space or hole) between two touching cells. This allows ions and molecules to move directly from one cell to another. Gap junctions are made up of connexin and other proteins. They are found in the epithelium of the skin but are also found in other tissue types such as s. Desmosomes act as molecular tethers that anchor epithelial cells to adjacent epithelial cells and the basement membrane. These junctions are made up of intermediate filaments and other fibrous and anchoring proteins. Spot desmosomes tie epithelial cells to one another whereas hemidesmosomes anchor the epithelium to the underlying basement membrane. These structures give epithelial tissue integrity and some resilience. Desmosomes can also be found in other tissue types such as cardiac muscle tissue. s prevent the paracellular (between cells) movement of substances by forming a tight seal between cells. These junctions can prevent any diffusion between cells or can provide some selective permeability. Tight junctions are made up of several types of integral (embedded in the cell membrane) proteins tied to the cytoskeleton.

Fig. 4.14: Types of
|
|
|
![]() Learning Outcomes
Learning Outcomes
- List the various types of exocrine gland secretions
- Describe the process of each type of secretion including degree of destruction to the cell.
Glandular Tissues
Glands can be either single cells or multicellular organs. They are primarily composed of epithelial tissues that secrete substances. s secrete endocrines (hormones). Endocrines (“endo-” = within) by definition are molecules that are secreted into the blood that influence tissues in another part of the body. Examples of endocrine glands include the thyroid gland and the adrenal glands. s, on the other hand, are an invaginated (infolded) epithelium with supporting connective tissue. The exocrine glands connect to the epithelial surface via a duct (epithelial-lined tube). Exocrine glands don’t just secrete individual molecules but often several molecules and ions along with a large water component. The exocrine glands secrete into a body compartment or out of the body (“exo-” = outside, to exit). Examples of exocrine glands include sweat glands and the glands that secrete digestive enzymes into the intestines.

Fig. 4.15: Types of exocrine gland with ducts
Exocrine glands are differentiated by how they secrete substances and where they are found in the human body (Figure). Merocrine glands package secretions into vesicles and release them through the typical exocytosis process you learned in Chapter 3. Examples of merocrine glands include lacrimal glands of the eyes, salivary glands of the oral cavity, pancreatic and gastric glands of the digestive system, and, most predominantly, sweat glands. Merocrine glands are the most common type of exocrine gland (mnemonic: “m” in merocrine stands for “most common”). Apocrine glands secrete by pinching off a piece of the plasma membrane. So the secretion contains cytoplasm and plasma membrane. Remember the plasma membrane is made up of predominantly phospholipids. So s are more oily (have more lipids) than the excretions of merocrine glands. These glands are found in the axillary and pelvic (pubic/anal) areas but also make up the mammary (breast) and ceruminous (ear) glands (mnemonic: “apo-” in apocrine stands for “axillary, pelvic, oily”). It has been recently discovered that some apocrine glands secrete using the merocrine process. Despite this axillary and pubic oil-secreting glands are still referred to as apocrine.
Finally, in holocrine glands, the epithelial cells completely disintegrate and are replaced by other mitotically (dividing) active cells. Therefore the secretions consist of the cell and all of the material inside of it (mnemonic: “holo-” stands for “the whole cell is part of the secretion”). Since lipids are part of this secretion, holocrine glands are oil-producing glands. Holocrine glands are the sebaceous (oil-producing) glands connected to hair follicles that coat the hair with oily sebum allowing them to grow through the follicle without becoming ingrown.

Fig. 4.16: Three models of glandular secretion.
| Gland Types: |
|
|
|
4.4 Connective Tissue
![]() Learning Outcomes
Learning Outcomes
- List the different types of connective tissue
- Describe the various types of cells that may be found in connective tissue and their function
- Describe the three different types of protein fibers found in connective tissue and list their properties
- Categorize the types of connective tissue based on their chemical composition, fiber arrangement and function
General Characteristics of Connective Tissue
Connective tissue has many specialized functions such as support, binding, and attachment of other tissues, protection of organs, energy storage, and body defenses against possible pathogens. Although the characteristics of connective tissue can vary widely, all connective tissues have 3 basic components: specialized connective tissue cells, extracellular protein fibers, and s. Unlike epithelial tissue where the cells make up the bulk of the tissue, connective tissue cells are far less numerous and not necessarily in contact with each other (Figure ). In other words, the specialized cells of connective tissue are surrounded by and suspended in the (the environment in which the cell lives). The matrix is a combination of the ground substance (a viscous, gel-like solution of water, ions, glycoproteins, and proteoglycans) and protein fibers. Imagine berries suspended and surrounded by jello. Specialized cells within the connective tissue secrete the ground substance and protein fibers (matrix) that encapsulate the cell. Many different types of specialized cells can be found in connective tissue discussed below.

Fig. 4.17: Connective Tissue Proper Fibroblasts produce this fibrous tissue. Connective tissue proper includes the fixed cells fibrocytes, adipocytes, and mesenchymal cells. LM × 400. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Cells Types of Connective Tissue
There is a specific formula for naming connective tissue cells. These cells are named for the connective tissue substance they produce. An immature connective tissue cell is more active at secreting matrix than the more mature connective tissue cell. These immature cells have blasts in their suffix. Mature, less active maintenance cells have cyte in their suffix. For example, connective tissue cells within loose and are called s or s. Cartilage cells are called chondroblasts or . Bone cells are osteoblasts or osteocytes and blood cells are hemocytoblasts or various -cytes that develop into red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes).
Other connective tissue cells are also found within the connective tissue matrix. Although these cells may not play an important role in forming the structure of connective tissue they help maintain the viability of the tissue. The properties of these cells are discussed below.
Fibroblasts are in abundance in the tissue and are actively secreting matrix. They secrete proteins and hyaluronan which combine to form the viscous proteoglycan previously mentioned. Fibroblasts are also active protein fiber producers. They actively produce collagen, elastic, or s, or a combination of the three.
A fibroblast will eventually mature and differentiate into a fibrocyte. Fibrocytes are less active matrix secreters, and function to monitor and maintain the matrix including existing protein fibers and are involved with tissue repair.
Macrophages are derived from a white blood cell known as a monocyte. They travel out of the bloodstream and make their way into connective tissues. Here they differentiate into even larger cells known as macrophages, literally known as “large eaters”. Macrophages may be fixed, residing in one place in the connective tissue or they may be free to wander throughout the connective tissue searching for any debris to remove. If they come upon debris or substances that they deem as foreign they are quickly activated to phagocytose the substance as well as release chemicals that activate other cells of the immune system.
Lymphocytes are also able to roam through connective tissue. They are also involved with the body’s defense system and provide the body with different types of immunity.
Mast cells are mobile cells that are also associated with the immune system. Mast cells are most numerous around blood vessels especially capillaries. They have a similar function to a type of white blood cell known as a basophil. An injured or infected sight will trigger the local mast cells to “dump” their numerous vesicles filled with and heparin. This exocytosis of histamine and heparin from the mast cell further stimulates the inflammatory response in tissue.
or fat cells are cells specialized to store large amounts of triglyceride. It is interesting to note that these cells have an almost limitless ability to expand to store more and more lipids because triglycerides are neutral fats and do not attract water into the cells. Adipocytes are found in different concentrations in various connective tissues ranging from none to making up the vast majority of the tissue bulk.
s are known as embryonic connective tissue cells. They can differentiate into various connective tissue cells.
Ground Substance and Protein Fibers (matrix)
The various connective tissue fibers all have unique properties and thus serve unique functions. The three CT fibers found in connective tissue are as follows:
is by far the most abundant type of fiber found in . Collagen is the result of three protein subunits called tropocollagen coiled together like a rope, thus it has rope-like characteristics. When these subunits are coiled together into a long, thick unbranching fiber it is referred to as type I collagen and has a great deal of strength. In other words, as with a rope, with many individual fibers wound together, collagen fibers together are very strong when pulled from end to end. This is referred to as having high tensile strength. With this property in mind, collagen fibers are ideal where there may be tissue subjected to pulling and high tension such as a tendon or ligament. Collagen fibers are usually easily identifiable under a microscope, they are larger than the other fibers and tend to stain pink in most prepared slides.
As the name implies, s are elastic. Containing the protein elastin, their properties can be compared to that of a bungee cord. When pulled from end to end elastic fibers will stretch and elongate. When released they will recoil. Elastic fibers tend to stain dark in histological samples and are found in tissues that are subjected to stretch. Elastic fibers are assembled on a precursor scaffolding made of a protein called fibrillin. In Marfan syndrome, there is a mutation in the gene that codes for this protein leading to weakened elastic fibers. People with Marfan syndrome tend to be tall and have long fingers and toes. It is suspected that Abraham Lincoln may have had Marfan syndrome. One unfortunate consequence of this disorder is a weakening of the aorta which can cause it to split, or dissect, which is often fatal.
Reticular fibers, or type III collagen, are uniquely different from either type I collagen or elastic fibers. These fibers are a different type of collagen assembled from the same tropocollagen subunits as type I collagen. However, unlike type I collagen, they form a delicate branching three-dimensional or scaffolding framework. This interwoven network or stroma creates a three-dimensional framework holding functional cells or in place giving organization to the cells of certain organs. A good example of where one would find reticular fibers is in , so-called due to the high concentration and organization supplied by the reticular fibers found there. This tissue can be found in the liver where cells (hepatocytes) need to be held in a particular arrangement near the blood supply and in the bone marrow, lymph nodes, and spleen.
![]() Cultural Connection
Cultural Connection
Weaving
Hilo, nahele paoa i ke ʻala.
Hilo, where the forest is imbued with fragrance.
Hilo’s forest is fragrant with hala and lehua blossoms.
ʻŌlelo Noʻeau, Collected by Mary Kawena Pukui (1983, 108 #1005)

A tissue performs unique functions that could not be done by cells alone or by other tissue types. Tissues are composed of specific cell types and acellular components, just like weaving a fishing net or cordage and the sail of a canoe from different plants. Hawaiians were master weavers and used different plant resources to weave and create materials to meet their needs. The Hala tree is one of the most important plants to Hawaiians. Its long, flexible, durable, and water-resistant lau was used to make the strong sails that brought kānaka (people) several thousand miles across the open ocean to Hawaiʻi. The lau are also used to make sleeping mats, sails, pillows, fans, and other items. Moena lau were coarse mats made with strips of lau hala an inch or wider. Moena makapepe used strips of a half-inch or less and were also used for floor mats. Moena pūʻao and moena makaliʻi were the finest mats and were used for bedding.
Hala is a native tree of Hawai’i. According to the moʻolelo, when Pele arrived on the shore of Hilo, she became entangled in the thorny leaves and roots of the hala trees. Pele became angry and tore up the trees and scattered them across the land. Each piece of hala that was scattered became a hala tree.
Connective Tissue Types
Embryonic connective tissue or mesenchymal tissue gives rise to the various tissues mentioned below. Mesenchymal cells are present in the developing embryo harboring the ability to differentiate into specific types of connective tissue cells. In adults, although the mesenchymal tissue is no longer present, the connective tissue will still contain mesenchymal stem cells that become active in tissue repair in the case of injury.
![]() Retrieval Practice
Retrieval Practice
Fill out the following chart from memory, then use the chapter to make corrections and fill in blanks

Connective Tissue Proper
Connective tissue proper is a classification of many different tissue types that are all produced by fibroblasts and contain various tissue properties. This classification can be first divided into loose and dense connective tissue. Here the terms “loose” and “dense” are referring to the degree to how densely packed the protein fibers appear under a microscope. There are three different types of both loose and dense connective tissue and their properties are discussed below.
Loose Connective Tissue
is divided into connective tissue proper types that have “loosely” packed fibers. They are as follows:
— Areola is Latin for “small space”. This is evident in areolar tissue where ground substance occupies the majority of the volume of the tissue which is permeated with loosely packed collagen, elastic and reticular fibers throughout. This allows the tissue to stretch and distort compensating for changes in volume and length. As it follows areolar tissue is sandwiched between the top and underlying layers of the skin as it allows the skin to move independently on top of deeper tissues such as muscle. It should be noted that areolar tissue provides an effective passageway and scaffolding for blood vessels. With this being said, areolar tissue provides a blood supply to and is commonly observed bordering underneath (deep to) the avascular epithelial tissue and, when functioning in this supportive role, is referred to as the .

Fig. 4.18: Areolar Tissue
— Adipose tissue contains the same protein fibers as areolar, however, the cells that make up the vast majority of the volume of adipose tissue are adipocytes, or fat cells. Having numerous fat cells allows adipose tissue to store energy in the form of lipids but the function of adipose tissue goes far beyond energy storage. Adipose is used as a “packing” material. It surrounds organs such as the delicate kidneys that are susceptible to shock or jarring. It is found around the heart, within the peritoneum of the abdominopelvic cavities, behind the eyeballs, and, of course, distributed in various places under the skin — buttocks, breasts, hips, etc.

Fig. 4.19: Adipose Tissue This is a loose connective tissue that consists of fat cells with little extracellular matrix. It stores fat for energy and provides insulation. LM × 800. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Reticular Tissue — Reticular tissue contains mostly the three-dimensional branching reticular fibers. As mentioned above reticular tissue forms a three-dimensional connective tissue framework or stroma for the functional cells, or parenchyma of an organ.

Fig. 4.20: Reticular Tissue This is a loose connective tissue made up of a network of reticular fibers that provides a supportive framework for soft organs. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Dense Connective Tissue
Dense connective tissue contains more collagen fibers than does loose connective tissue. As a consequence, it has greater resistance to stretching. There are two major categories of dense connective tissue.
Dense Regular Connective Tissue [Figure 4.21] As the name implies, dense regular connective tissue has densely packed fibers (collagen) that are arranged in a regular fashion. In other words, if you observe a slide of dense regular connective tissue you will find that the vast majority of the volume of this tissue is taken up by collagen fibers that are, for the most part, running parallel with each other. Notice from the image that the collagen fibers are very densely packed and all running in a parallel fashion. As you may expect this type of tissue with such tightly packed collagen has high tensile strength. This is the preferred tissue to use when there is a lot of strain when pulling from end to end such as what happens on a tendon or ligament. A tendon connects muscle to bone and a ligament connects bone to bone. Appreciate the immense amount of tension that may be put on either tendon or ligament. Think of a powerlifter bench pressing 700 lbs. The tendons that connect the major chest muscle pectoralis major to the humerus are under tremendous strain. The collagen fibers that make up ligaments are so strong that in many instances, under tremendous strain, a tendon will rip off a chunk of the bone before tearing itself. This is known as an avulsion fracture.
Dense Irregular Connective Tissue Dense irregular connective tissue is permeated with mostly collagen fibers. However, unlike dense regular CT., the collagen fibers are not parallel to one another, they are dispersed in the tissue in random directions. This interwoven meshwork of collagen fibers provides strength when the tissue is being pulled in various directions. The skin, for example, can be pulled back and forth and sideways as the limbs are moved. Dense irregular connective tissue comprises a major part of the dermis, the layer of the skin below the epidermis. Further, dense irregular connective tissue is found surrounding portions of bones, cartilage, joint, and organ capsules.

Fig. 4.21: Dense regular and dense irregular connective tissue. (a) Dense regular connective tissue consists of collagenous fibers packed into parallel bundles. (b) Dense irregular connective tissue consists of collagenous fibers interwoven into a mesh-like network. From top, LM × 1000, LM × 200. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
Elastic Connective Tissue Elastic tissue contains densely packed arrangements of elastic fibers. This tissue is found in areas that require some elasticity allowing for movement such as the elastic ligaments that are found running up and down the vertebral column.

Fig. 4.22 Elastic Connective Tissue

Fluid Connective Tissues
![]() 4.2 Learning Outcomes
4.2 Learning Outcomes
- List the different types of fluid connective tissue
- Describe the properties of blood
- Describe the properties of lymph
The role of connective tissues is to connect and support all of the other tissues. So it may be surprising to some of you that blood is connective tissue. Blood connective tissue physically connects all the tissues together, not by acting as an anchor or support as with the other connective tissues but by distributing nutrients and removing waste products. Oxygen is distributed throughout the body carried by RBCs (red blood cells, aka erythrocytes (“red cells”)). The blood also plays an important role in your immune system by helping to distribute WBCs (white blood cells, aka leukocytes (“white cells”)) which move about our tissues looking for foreign substances to destroy and to mount immune responses against. Also found in the blood are platelets (thrombocytes (“ cells”)) which help plug holes in damaged blood vessels (blood clotting). Because erythrocytes and platelets are not complete cells, RBCs, WBCs, and platelets are collectively called the formed elements of the blood.
Aside from the formed elements, there is also a major fluid component to the blood. This fluid part of the blood is called plasma (fluid-like). The blood plasma contains dissolved proteins, nutrients, wastes, hormones, and ions. Unlike typical connective tissue, the protein of blood is not insoluble protein fibers, but rather dissolved globular proteins within the watery matrix of the plasma.

Fig. 4.23 Blood: A Fluid Connective Tissue Blood is a fluid connective tissue containing erythrocytes and various types of leukocytes that circulate in a liquid extracellular matrix. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
The blood is not the only . Lymph is an acellular (no cells) fluid connective tissue found in the lymphatic system, a vascular system separate from the blood’s cardiovascular system. The lymphatic system helps return plasma that moved from capillaries to the tissues but did not reenter capillaries at the venous end (relating to veins). Lymph gets filtered through a series of lymph nodes to remove foreign particles and mount immune responses before it is returned to the cardiovascular system as plasma.
 |

|
| Cardiovascular System | Lymphatic System |
Fig. 4.24 Comparing the cardiovascular system and the lymphatic system
Supportive Connective Tissues
![]() 4.3 Learning Outcomes
4.3 Learning Outcomes
- List the various types of supporting connective tissue and their functions
- Describe the functions of cells making up supporting connective tissue
- List the supporting connective tissue that is vascular vs. avascular
Some connective tissues serve to support the body by providing a framework and by anchoring various tissues and organs together. Osseous (bone) connective tissue provides a framework for the body and assists with weight bearing. Bones also provide anchor sites for muscles providing movement. Osseous tissue contains osteocytes (bone cells) but unlike other connective tissues, the ground matrix is a dense, hardened material containing calcium-phosphate crystals covering a helical arrangement of collagen called osteoid. The osteocytes live in lacuna (little pockets) within the hardened osteoid. There are two different types of bone tissue. Spongy bone looks like a sponge; it is very porous (has many holes or spaces). The other osseous tissue is the compact bone which is very dense (no pores). Spongy bone is found on the interior of bone organs, whereas compact bone is found on the exterior regions and provides most of the strength. Compact bone is made of cylindrical structures called osteons which are made of many circular plate-like layers (lamellae). In addition to providing a framework and lever system for the muscles to pull. . Bone also protects vital organs, stores minerals and performs hemopoietic (hematopoiesis, the making of blood cells) functions. “Osteo-” and “Osseo-” are prefixes that refer to bone tissue or organs.
Cartilage is also a supporting connective tissue. The ground matrix of cartilage is between that of blood and bone; it is a semisolid extracellular (outside of cells) matrix. Collagen and elastic protein fibers are present along with chondrocytes (cartilage cells) that, as with bone cells, live in pockets called . Cartilage is sometimes surrounded by a dense irregular CT covering called the perichondrium (around the cartilage) which includes both an outer fibrous layer and inner cellular layer. Cartilage is stronger and more resilient than other connective tissues except for bone. However, cartilage is more flexible than bone and so occurs in areas of your body that need support but must withstand deformation (e.g., the tip of the nose).
When fully mature, cartilage is avascular (without vasculature, no blood vessels) and is therefore slow to heal from injury. This is the only type of connective tissue that is avascular. There are three types of cartilage: hyaline cartilage, , and (Figure 4.25). is the most common type. Under the microscope, hyaline has a clear glassy appearance with scattered cells in their lacunae. It can be found in the nose, trachea, larynx, costals (ribs) and the articular (joint-forming) ends of long bones. Fibrocartilage are dense weight- and shock-absorbing pads found throughout the body. More numerous parallel type I collagen fibers within the ground matrix provide the necessary resilience to resist compression. Fibrocartilage is found in intervertebral discs, the pubic symphysis, and menisci of the knee and other joints. Elastic cartilage is flexible due to more elastic fibers and fewer collagen fibers. Elastic cartilage, when stretched, can recoil (return to its original shape). Chondrocytes are more numerous and the ground matrix appears a dark purple in microscope images. Elastic cartilage is found in the external ear and the epiglottis.

Fig. 4.25: Types of Cartilage Cartilage is a connective tissue consisting of collagenous fibers embedded in a firm matrix of chondroitin sulfates. (a) Hyaline cartilage provides support with some flexibility. The example is from dog tissue. (b) Fibrocartilage provides some compressibility and can absorb pressure. (c) Elastic cartilage provides firm but elastic support. From top, LM × 300, LM × 1200, LM × 1016. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
4.5 Muscle Tissue
![]() 4.5 Learning Outcomes
4.5 Learning Outcomes
- List the various types of muscle tissue and functions of each
Muscle tissue is mainly characterized by its ability to contract. There are three types of muscle tissues; , cardiac muscle, and . Muscle cells also known as muscle fibers are long slender, cylinder-shaped cells with s (stripes) created by the overlapping contractile proteins. During embryonic development, these cells arise from multiple germ cells fusing together, hence these cells are multinucleate (contain many nuclei). As a tissue, these cells are parallel (aligned along their broadsides). Skeletal muscle tissues attach to and pull on bones to move the body. Since we generally think of bodily movement as being consciously or deliberately controlled, skeletal muscle tissue is often described as voluntary. Cardiac muscle tissue is only found in the heart. The cells are also striated but instead of being long parallel cylinders, they are branched. They are also uninucleated instead of multinucleated. This muscle tissue surrounds chambers of the heart causing them to contract and pumping blood around the body. Since you do not have to consciously remind your heart to beat this type of muscle is considered involuntary (not voluntary). Smooth muscles are found in the walls of hollow organs such as your G.I. (gastrointestinal), respiratory, and reproductive tracts and also in the pupils of the eye and the arrector pili muscles attached to the hairs in your skin. These muscle cells are spindle-shaped (fusiform, pointed at both ends) and non-striated (no stripes). As with cardiac muscle, this type of muscle is also involuntary and uninucleated.

Fig. 4.26: Types of Muscle Tissue: Smooth muscle, cardiac muscle, and skeletal muscle
4.6 Nervous Tissues
![]() 4.6 Learning Outcomes
4.6 Learning Outcomes
- Describe the function of nervous tissue and various types of involved.
Nervous tissues respond to various stimuli which can result in the stimulation of other nervous tissues, contraction of muscles, and/or gland secretion. s are the functional cell type of nervous tissues (Figure 4.27). These cells have a distinct soma (body) with projecting dendrites (finger-like processes) and a long thin axon. The end of the axon is called the axon terminus (where the axon terminates). The soma and dendrites react to stimuli by initiating electrical signals that spread down the axon causing the release of a chemical called a neurotransmitter from the terminus. Neurotransmitters transmit signals to other neurons, muscle tissue, or glands. Although neurons are the functional cells of nervous tissue, they are maintained by the more numerous or glial cells that support, nourish, and bind neurons together. There are several types of neuroglial cells. The details of how neurons function and the various types of neuroglial cells are covered in Chapter 9.

Fig. 4.27: Neuron The cell body of a neuron, also called the soma, contains the nucleus and mitochondria. The dendrites transfer the nerve impulse to the soma. The axon carries the action potential away to another excitable cell. LM × 1600. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
As a review, tissues are groups of similar cells serving a common function. You learned the four main types of tissues.
|
|
|
|
Organs, on the other hand, are composed of groups of different tissues grouped together serving a common function. For instance, muscle cells group together to form muscle tissues that allow for body movement. Muscle organs are muscle tissues combined with other tissue types (epithelium, nervous and connective). These other tissues provide the nutrients, control, and anchoring structures required for the muscle organ to work properly. For example, the heart is an organ. It consists mostly of cardiac muscle but contains (the epithelium of blood vessels), nervous tissue (controls the heart rate and contraction force), and connective tissues (holds it all together). Bones are also organs and are not just osseous (bone) tissue. Like the heart, skeletal bones contain other tissue types too.
4.7 Body Membranes
Body membranes are thin, sheet-like structures made up of epithelial tissues with underlying connective tissues. These membranes line or cover body cavities, viscera (organs), and the external surface (aka the skin) (Figure x).
Mucous membranes, often called the mucosa, line compartments that are exposed to the outside environment such as the digestive, respiratory, urinary, and reproductive tracts. These membranes perform adsorption and secretory functions in addition to protecting the underlying tissues. The connective tissue component is referred to as the lamina (plate-like) propria (common property). The epithelial tissues include mucus-secreting goblet cells scattered amongst the epithelial cells and/or multicellular mucus-secreting glands in the submucosal connective tissue attached to the surface by ducts. Mucin is a glycoprotein that combines with water to produce mucus which makes the surface of these mucous membranes slippery and slimy and protects the tissues from abrasion and dangerous substances or microorganisms.
s line body cavities not exposed to the outside environment such as the abdominopelvic or peritoneal cavity (peritoneal serous membranes), pleural cavity (pleural serous membranes), and pericardial cavity (pericardial serous membranes). Serous membranes fold so that two layers are covering the organ. The layer closest to the organ or viscera is called the visceral layer. The layer on the outside that lines the cavity is called the parietal layer. These membranes are made of a simple squamous epithelial layer called that produces serous fluid. This fluid is secreted into the serous cavity (the space between the folds of the membrane). The serous fluid reduces friction between the organs preventing damage through wear and tear and unnecessary heat generation.
s line synovial joint cavities of the body. Unlike the other membranes with an epithelium, these membranes are composed of areolar connective tissue. The membranes produce synovial fluid which helps to nourish the avascular articular cartilage covering the ends of the long bones and also creating a slippery surface for the bones to glide over one another during movements.
Cutaneous membranes (the skin or integument) are the subject of the next chapter. These membranes cover the surface of the human body. It is referred to as keratinized stratified squamous epithelium since these membranes generate a lot of the protein keratin. These membranes also include an underlying connective tissue layer (dermis). The skin is the largest organ of the body and serves to protect against infection, loss of water and is also the body’s largest sensory organ.

Fig. 4.28: Tissue Membranes The two broad categories of s in the body are (1) s, which include synovial membranes, and (2) s, which include mucous membranes, serous membranes, and the cutaneous membrane, in other words, the skin.
4.8 Understand How Tissues Change in Health and Disease
![]() 4.8 Learning Outcomes
4.8 Learning Outcomes
- Discuss how the generalized cells of a developing embryo or the stem cells of an adult organism become differentiated into specialized cells
- Distinguish between the categories of stem cells
All humans start as a single cell called a zygote which is created when the male sperm and female ovum fuse together. During the early stages of tissue development, the zygote divides in several stages to become a blastocyst and then an embryoblast. The embryoblast produces three cell layers called the primary germ layers: , , and . These layers will differentiate into all the various tissues of the body.

Fig. 4.29: Embryoblast
How does one cell become all the various tissues of the body? Early developed cells are called stem cells. because they can differentiate (change) into other cell types. Once a cell differentiates it can’t reverse back to an earlier stage of development. The zygote is an omnipotent or (total potency) cell that can divide to form any other cell type within the embryo or placenta. Pluripotent stem cells (“pluri-” = many) can change into any cell type other than the placenta. Multipotent stem cells are limited in their capacity to differentiate but can change into many other cell types. You can find multipotent stem cells in the bone marrow, these cells can differentiate into any blood cell type. Unipotent stem cells can divide to form one other cell type. Finally, terminally differentiated cells can form one cell type. Liver cells, or hepatocytes, for example, divide to form other hepatocytes but cannot become blood cells. As the embryo develops the cells of the primitive germ layers differentiate. The cells of the ectoderm form nervous tissue and the epithelium of the skin. The endoderm forms the epithelium lining the gastrointestinal and respiratory tracts and the mesoderm forms all of the connective tissue, the lining of the blood vessels and muscles of the body.

Fig. 4.30: Different types of human cells with various sizes, shapes, and functions.

Figure 4.31: Stem Cells: The capacity of stem cells to differentiate into specialized cells makes them potentially valuable in therapeutic applications designed to replace damaged cells of different body tissues.
Sometimes tissues change in appearance due to normal developmental processes or in response to insult or injury. Hypertrophy (“-trophy” = growth) is when tissue cells increase in size but not in number. However, if cells increase in number (they are multiplying) it is called hyperplasia (“-plasia” = cell multiplication). is the shrinkage of tissue either due to loss of cell numbers or size. All of the above can be caused by normal/healthy physiological processes. For instance, inactivity causes the atrophy of skeletal muscles.

Figure 4.32: Epithelium
Tissue changes can occur due to some sort of stimuli such as injury or other pathology. If a tissue morphology (appearance, shape) changes it is called metaplasia. Sometimes metaplasia is a normal developmental process but other times it is a response to a damaging stimulus. For example, in people who regularly smoke their normal pseudostratified epithelium changes into the stratified squamous keratinized epithelium. The stratification (multiple layers) of this tissue helps protect the underlying tissues from the chemicals and heat of the inhaled smoke. Another example is when the stratified squamous epithelium of the esophagus responds to acid refluxing from the stomach by transitioning into gastric mucosa as a protective response. When metaplasia occurs due to a pathological process there is a risk for cells changing in a way that is a precursor to cancer. This is called dysplasia. Neoplasia is when tissue has changed its characteristics and growth becomes unregulated. This may cause a benign tumor (localized growth, not spreading) or malignant cancer. Malignant cancers are dangerous because the rapidly multiplying cells begin to metastasize (spread around the body to other tissues) which interferes with normal physiology.
describes tissue death due to irreparable damage. This can be a result of insult or injury or caused by other factors. Gangrene is necrosis of a tissue due to loss of blood supply to a tissue. The most common sites are the fingers and toes but can occur in other areas of the body as well. Another form of tissue death is caused by or programmed cell death. This is a more orderly form of cell death that does not result in inflammation and is sometimes a normal part of development, such as when we lose the webbing between our fingers and toes as a fetus.
|
|
|
|

Fig. 4.33: Gangrene
With proper nutrition, good health and blood circulation and infrequent injuries tissues can more or less stay the same over decades of life. However, as we age mitosis (cell division) and repair of tissues become less efficient. This results in epithelial lining thinning, connective tissues losing plasticity and resilience (strength, resistance to change), bones become more brittle due to a decline in collagen production, and muscle atrophy.

Chapter Summary

Key Terms
adipocytes
lipid storage cells
adipose tissue
specialized areolar tissue dominated by adipocytes
apical
that part of a cell or tissue which, in general, faces an open space
apocrine secretion
release of a substance along with the apical portion of the cell
apoptosis
programmed cell death
areolar tissue
(also, loose connective tissue) a type of connective tissue proper that shows little specialization with cells dispersed in the matrix
atrophy
loss of mass and function
basal lamina
thin extracellular layer that lies underneath epithelial cells and separates them from other tissues
basement membrane
in epithelial tissue, a thin layer of fibrous material that anchors the epithelial tissue to the underlying connective tissue; made up of the basal lamina and reticular lamina
cardiac muscle
heart muscle, under involuntary control, composed of striated cells that attach to form fibers, each cell contains a single nucleus, contracts autonomously
cell junction
point of cell-to-cell contact that connects one cell to another in a tissue
chondrocytes
cells of the cartilage
clotting
also called coagulation; complex process by which blood components form a plug to stop bleeding
collagen fiber
flexible fibrous proteins that give connective tissue tensile strength
connective tissue
type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems
connective tissue membrane
connective tissue that encapsulates organs and lines movable joints
connective tissue proper
connective tissue containing a viscous matrix, fibers, and cells.
cutaneous membrane
skin; epithelial tissue made up of a stratified squamous epithelial cells that cover the outside of the body
dense connective tissue
connective tissue proper that contains many fibers that provide both elasticity and protection
ectoderm
outermost embryonic germ layer from which the epidermis and the nervous tissue derive
elastic cartilage
type of cartilage, with elastin as the major protein, characterized by rigid support as well as elasticity
elastic fiber
fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fibers to stretch and return to original size
endocrine gland
groups of cells that release chemical signals into the intercellular fluid to be picked up and transported to their target organs by blood
endoderm
innermost embryonic germ layer from which most of the digestive system and lower respiratory system derive
endothelium
tissue that lines vessels of the lymphatic and cardiovascular system, made up of a simple squamous epithelium
epithelial membrane
epithelium attached to a layer of connective tissue
epithelial tissue
type of tissue that serves primarily as a covering or lining of body parts, protecting the body; it also functions in absorption, transport, and secretion
exocrine gland
group of epithelial cells that secrete substances through ducts that open to the skin or to internal body surfaces that lead to the exterior of the body
fibroblast
most abundant cell type in connective tissue, secretes protein fibers and matrix into the extracellular space
fibrocartilage
tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance
fibrocyte
less active form of fibroblast
fluid connective tissue
specialized cells that circulate in a watery fluid containing salts, nutrients, and dissolved proteins
gap junction
allows cytoplasmic communications to occur between cells
goblet cell
unicellular gland found in columnar epithelium that secretes mucous
ground substance
fluid or semi-fluid portion of the matrix
histamine
chemical compound released by mast cells in response to injury that causes vasodilation and endothelium permeability
histology
microscopic study of tissue architecture, organization, and function
hyaline cartilage
most common type of cartilage, smooth and made of short collagen fibers embedded in a chondroitin sulfate ground substance
inflammation
response of tissue to injury
lacunae
(singular = lacuna) small spaces in bone or cartilage tissue that cells occupy
lamina propria
areolar connective tissue underlying a mucous membrane
loose connective tissue
(also, areolar tissue) type of connective tissue proper that shows little specialization with cells dispersed in the matrix
matrix
extracellular material which is produced by the cells embedded in it, containing ground substance and fibers
mesenchymal cell
adult stem cell from which most connective tissue cells are derived
mesoderm
middle embryonic germ layer from which connective tissue, muscle tissue, and some epithelial tissue derive
mesothelium
simple squamous epithelial tissue which covers the major body cavities and is the epithelial portion of serous membranes
mucous membrane
tissue membrane that is covered by protective mucous and lines tissue exposed to the outside environment
muscle tissue
type of tissue that is capable of contracting and generating tension in response to stimulation; produces movement.
necrosis
accidental death of cells and tissues
nervous tissue
type of tissue that is capable of sending and receiving impulses through electrochemical signals.
neuroglia
supportive neural cells
neuron
excitable neural cell that transfer nerve impulses
parenchyma
functional cells of a gland or organ, in contrast with the supportive or connective tissue of a gland or organ
pseudostratified columnar epithelium
tissue that consists of a single layer of irregularly shaped and sized cells that give the appearance of multiple layers; found in ducts of certain glands and the upper respiratory tract
reticular fiber
fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue
reticular tissue
type of loose connective tissue that provides a supportive framework to soft organs, such as lymphatic tissue, spleen, and the liver
serous membrane
type of tissue membrane that lines body cavities and lubricates them with serous fluid
simple columnar epithelium
tissue that consists of a single layer of column-like cells; promotes secretion and absorption in tissues and organs
simple cuboidal epithelium
tissue that consists of a single layer of cube-shaped cells; promotes secretion and absorption in ducts and tubules
simple squamous epithelium
tissue that consists of a single layer of flat scale-like cells; promotes diffusion and filtration across surface
skeletal muscle
usually attached to bone, under voluntary control, each cell is a fiber that is multinucleated and striated
smooth muscle
under involuntary control, moves internal organs, cells contain a single nucleus, are spindle-shaped, and do not appear striated; each cell is a fiber
stratified columnar epithelium
tissue that consists of two or more layers of column-like cells, contains glands and is found in some ducts
stratified cuboidal epithelium
tissue that consists of two or more layers of cube-shaped cells, found in some ducts
stratified squamous epithelium
tissue that consists of multiple layers of cells with the most apical being flat scale-like cells; protects surfaces from abrasion
striation
alignment of parallel actin and myosin filaments which form a banded pattern
synovial membrane
connective tissue membrane that lines the cavities of freely movable joints, producing synovial fluid for lubrication
tight junction
forms an impermeable barrier between cells
tissue
group of cells that are similar in form and perform related functions
tissue membrane
thin layer or sheet of cells that covers the outside of the body, organs, and internal cavities
totipotent
embryonic cells that have the ability to differentiate into any type of cell and organ in the body
transitional epithelium
form of stratified epithelium found in the urinary tract, characterized by an apical layer of cells that change shape in response to the presence of urine
Sources
http://www.kumukahi.org/units/na_kanaka/oihana/ulana_lau_hala
Media Attributions
- olelo_noeau
- Connective_Tissue_Tendon_(41812677172) © Berkshire Community College Bioscience Image Library is licensed under a CC0 (Creative Commons Zero) license
- Epithelial_Tissues_Simple_Squamous_Epithelium_(frog)_(27847646938) © Berkshire Community College Bioscience Image Library is licensed under a CC0 (Creative Commons Zero) license
- Muscle_Tissue_Cross_Section_Whole_Skeletal_Muscle_(41241955204) © Berkshire Community College Bioscience Image Library is licensed under a CC0 (Creative Commons Zero) license
- Nervous_Tissue_Nerve_Bundle_(40110796600) © Berkshire Community College Bioscience Image Library is licensed under a CC0 (Creative Commons Zero) license
- 4 Types of Tissue POC © LOUIS: The Louisiana Library Network is licensed under a CC BY (Attribution) license
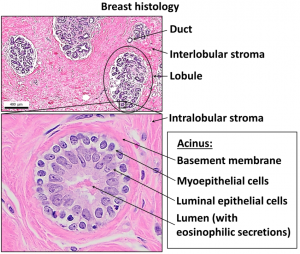
- Normal breast histology – Simple squamous epithelium with basement membrane © Mikael Häggström, M.D. is licensed under a CC BY (Attribution) license
- Cellular tight junction keys © LadyofHats adapted by LLys is licensed under a Public Domain license
- Goblet Cell a © Openstax is licensed under a CC BY (Attribution) license
- Goblet Cell b © Openstax is licensed under a CC BY (Attribution) license
- Summary Epithelial Tissue Cells © Openstax is licensed under a CC BY (Attribution) license
- Simple Squamous Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Simple Cuboidal Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Simple Columnar Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Stratified Squamous Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Stratified Cuboidal Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Stratified Columnar Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Pseudostratified Columnar Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Transitional Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Types Cell Junctions © Openstax is licensed under a CC BY (Attribution) license
- Types of Exocrine Gland with Duct © Openstax is licensed under a CC BY (Attribution) license
- Three Models Glandular Secretion © Openstax is licensed under a CC BY (Attribution) license
- Connective Tissue Proper © Openstax, Regents of University of Michigan Medical School is licensed under a CC BY (Attribution) license
- Lauhala_weaver,_Pukoo,_Molokai_(PP-33-6-001) © Ray Jerome Baker (1880–1972) is licensed under a Public Domain license
- Tissue Fill Out Chart © UH A&P is licensed under a CC BY (Attribution) license
- Connective_Tissue_Loose_Aerolar_(41743649122) © Author Berkshire Community College Bioscience Image Library is licensed under a CC0 (Creative Commons Zero) license
- Adipose Tissue © Openstax is licensed under a CC BY (Attribution) license
- Reticular Tissue © Openstax is licensed under a CC BY (Attribution) license
- Dense Connective Tissue 9k © Openstax is licensed under a CC BY (Attribution) license
- STD_190219_SWITCH_Tissue_2_93x_CMLE_20SNR_50IT_Elastin © Howard Vindin is licensed under a CC BY-SA (Attribution ShareAlike) license
- Elastic Connective Tissues © Oregon State University is licensed under a CC BY-SA (Attribution ShareAlike) license
- Blood Fluid Connective Tissue © Openstax is licensed under a CC BY (Attribution) license
- Circulatory_System_en © LadyofHats Mariana Ruiz Villarreal is licensed under a Public Domain license
- Lymphatic System © Openstax is licensed under a CC BY (Attribution) license
- Types of Cartilage © Openstax is licensed under a CC BY (Attribution) license
- Types_Of_Muscle © www.scientificanimations.com is licensed under a CC BY-SA (Attribution ShareAlike) license
- The Neuron © Openstax is licensed under a CC BY (Attribution) license
- Tissue Membranes © Openstax is licensed under a CC BY (Attribution) license
- Embryoblast © Openstax is licensed under a CC BY (Attribution) license
- Final_stem_cell_differentiation_(1) © Haileyfournier is licensed under a CC BY-SA (Attribution ShareAlike) license
- Stem Cells © Openstax is licensed under a CC BY (Attribution) license
- Epithelium © Openstax is licensed under a CC BY (Attribution) license
- Wiki GangreneFoot © James Heilman, MD is licensed under a CC BY-SA (Attribution ShareAlike) license
- Honu_‘Iwalani Clayton_CCBY_2022 10 30 © ‘Iwalani Clayton is licensed under a CC BY (Attribution) license
- divider_maile
An aggregate of similar cells and cell products forming a definite kind of structural material.
Type of tissue that serves primarily as a covering or lining of body parts, protecting the body; it also functions in absorption, transport, and secretion.
Type of tissue that serves to hold in place, connect, and integrate the body’s organs and systems.
Type of tissue that is capable of contracting and generating tension in response to stimulation; produces movement.
Type of tissue that is capable of sending and receiving impulses through electrochemical signals.
Microscopic study of tissue architecture, organization, and function.
Skin; epithelial tissue made up of a stratified squamous epithelial cells that cover the outside of the body.
in epithelial tissue, a thin layer of fibrous material that anchors the epithelial tissue to the underlying connective tissue; made up of the basal lamina and reticular lamina
Thin extracellular layer that lies underneath epithelial cells and separates them from other tissues.
That part of a cell or tissue which, in general, faces an open space.
Tissue membrane that is covered by protective mucous and lines tissue exposed to the outside environment.
Unicellular gland found in columnar epithelium that secretes mucous.
Tissue that consists of a single layer of flat scale-like cells; promotes diffusion and filtration across surface.
Tissue that consists of a single layer of cube-shaped cells; promotes secretion and absorption in ducts and tubules.
Tissue that consists of a single layer of column-like cells; promotes secretion and absorption in tissues and organs.
Tissue that consists of multiple layers of cells with the most apical being flat scale-like cells; protects surfaces from abrasion.
Tissue that consists of two or more layers of cube-shaped cells, found in some ducts.
Tissue that consists of two or more layers of column-like cells, contains glands and is found in some ducts.
Tissue that consists of a single layer of irregularly shaped and sized cells that give the appearance of multiple layers; found in ducts of certain glands and the upper respiratory tract.
Form of stratified epithelium found in the urinary tract, characterized by an apical layer of cells that change shape in response to the presence of urine.
Allows cytoplasmic communications to occur between cells.
Heart muscle, under involuntary control, composed of striated cells that attach to form fibers, each cell contains a single nucleus, contracts autonomously.
Forms an impermeable barrier between cells.
Point of cell-to-cell contact that connects one cell to another in a tissue.
Groups of cells that release chemical signals into the intercellular fluid to be picked up and transported to their target organs by blood.
Group of epithelial cells that secrete substances through ducts that open to the skin or to internal body surfaces that lead to the exterior of the body.
Release of a substance along with the apical portion of the cell.
Fluid or semi-fluid portion of the matrix.
Extracellular material which is produced by the cells embedded in it, containing ground substance and fibers.
Connective tissue proper that contains many fibers that provide both elasticity and protection.
Most abundant cell type in connective tissue, secretes protein fibers and matrix into the extracellular space.
Less active form of fibroblast.
Cells of the cartilage.
Fine fibrous protein, made of collagen subunits, which cross-link to form supporting “nets” within connective tissue.
Chemical compound released by mast cells in response to injury that causes vasodilation and endothelium permeability.
Lipid storage cells.
Adult stem cell from which most connective tissue cells are derived.
Flexible fibrous proteins that give connective tissue tensile strength.
Connective tissue containing a viscous matrix, fibers, and cells.
Fibrous protein within connective tissue that contains a high percentage of the protein elastin that allows the fibers to stretch and return to original size.
Functional cells of a gland or organ, in contrast with the supportive or connective tissue of a gland or organ.
Type of loose connective tissue that provides a supportive framework to soft organs, such as lymphatic tissue, spleen, and the liver.
(Also, areolar tissue) type of connective tissue proper that shows little specialization with cells dispersed in the matrix.
(Also, loose connective tissue) a type of connective tissue proper that shows little specialization with cells dispersed in the matrix.
Areolar connective tissue underlying a mucous membrane.
Specialized areolar tissue dominated by adipocytes.
Also called coagulation; complex process by which blood components form a plug to stop bleeding.
Specialized cells that circulate in a watery fluid containing salts, nutrients, and dissolved proteins.
(Singular = lacuna) spaces in a bone that house an osteocyte.
Tough form of cartilage, made of thick bundles of collagen fibers embedded in chondroitin sulfate ground substance.
Type of cartilage, with elastin as the major protein, characterized by rigid support as well as elasticity.
Most common type of cartilage, smooth and made of short collagen fibers embedded in a chondroitin sulfate ground substance.
Usually attached to bone, under voluntary control, each cell is a fiber that is multinucleated and striated.
Under involuntary control, moves internal organs, cells contain a single nucleus, are spindle-shaped, and do not appear striated; each cell is a fiber.
Alignment of parallel actin and myosin filaments which form a banded pattern.
Excitable neural cell that transfer nerve impulses.
Supportive neural cells.
Tissue that lines vessels of the lymphatic and cardiovascular system, made up of a simple squamous epithelium.
Membrane that covers organs and reduces friction; also referred to as serosa.
Simple squamous epithelial tissue which covers the major body cavities and is the epithelial portion of serous membranes.
Connective tissue membrane that lines the cavities of freely movable joints, producing synovial fluid for lubrication.
Thin layer or sheet of cells that covers the outside of the body, organs, and internal cavities.
Connective tissue that encapsulates organs and lines movable joints.
Epithelium attached to a layer of connective tissue.
Outermost embryonic germ layer from which the epidermis and the nervous tissue derive.
Middle embryonic germ layer from which connective tissue, muscle tissue, and some epithelial tissue derive.
Innermost embryonic germ layer from which most of the digestive system and lower respiratory system derive.
Embryonic cells that have the ability to differentiate into any type of cell and organ in the body.
Loss of mass and function.
Accidental death of cells and tissues.
Response of tissue to injury.
Programmed cell death.




