Anatomy and Physiology
6 Osseous Tissue
 Ola nā iwi
Ola nā iwi
The bones live.
Said of a respected oldster who is well cared for by his family.
‘Ōlelo No‘eau, compiled by Mary Kawena Pukui, #2488
Introduction
Fig 6.1: Video of Hawaiian bone carving
![]() Chapter Learning Outcomes
Chapter Learning Outcomes
- Describe bone physiology
- Describe osseous tissue microanatomy and macro anatomy
- List and describe the other tissues associated with bone organs
- List and name one bone of each shape classification
- Indicate the physiological roles of calcium, collagen, and vitamins C and D
- Describe the different types of bone tissue development and growth
- List several human skeleton diseases and fracture types
- Describe the stages of the healing process
or is a supportive connective tissue. It consists of approximately one-third organic content, including collagen fibers and ground substance, and two-thirds inorganic content, including various calcium phosphate salts, but it also contains various living “breathing” cells that need a continuous blood supply.
The delivery of oxygen and nutrients and the removal of waste products to the various bone cells is a major theme in understanding the microanatomy of osseous tissue. Even though bone is a solid matrix there are passageways throughout that allow blood vessels to deliver a steady stream of nutrients and remove wastes from the tissue.
One of the main functions of bone is to provide attachment points for skeletal muscles. As the muscles pull on the bones, this creates bumps or processes along the surface. As skeletal muscles contract, they pull on bones to produce various body movements. For each skeletal muscle that pulls bones in one direction, there must be another muscle to move the bones in the opposite direction. Providing body movement isn’t the only function of the . There are many other physiological functions that the skeletal system provides.
6.1 General Functions of Bone
![]() 6.1 Learning Outcomes
6.1 Learning Outcomes
- Describe the role bones play in body movement
- Describe how bones support and protect organs of the body
- List the types of bone marrow and describe the physiological roles of each
Movement: As you will learn in later chapters, the musculoskeletal system is a highly complex pulley system allowing movement based on the arrangement and attachment of skeletal muscles to bones.
Support and Protection: Bones of the skeletal system provide a structural framework for protection and stability with other organs found throughout the body. The bones of the cranium and rib cage are obvious examples of this and demonstrate how form dictates function. These bones encase, and therefore protect, the underlying organs.
: Red bone marrow within the medullary region of bones in children and certain s of adults are responsible for the production of all blood cells (both red blood cells, white blood cells, and platelets). Red blood cells (RBCs) carry oxygen to various tissues, white blood cells (WBCs) help fight infection, and platelets help with blood clotting. These concepts will be discussed in detail in the chapters covering blood and the immune system.
Storage of minerals and lipids: Yellow bone marrow plays a role in the storage of certain minerals and lipids. In this chapter, you will learn that the bone matrix is primarily composed of calcium and phosphate ions in combination with collagen fibers. These calcium phosphate salts crystalize, imparting bone with hardness but also serving as a storage depot for these ions. If blood calcium or phosphate is low, the bone matrix will be broken down, providing these salts to the rest of the body, and if the blood concentration is high, they can be deposited into the bone matrix. Long bones have hollow spaces called medullary cavities filled with high concentrations of adipose tissue containing high quantities of triglycerides. These molecules serve as an energy reservoir that can be mobilized when needed.
| Table of Bone Functions |
| 1. Movement |
| 2. Support and protection |
| 3. Hematopoiesis |
| 4. Mineral and lipid storage |
6.2 Types of Bone
![]() 6.2 Learning Outcomes
6.2 Learning Outcomes
- Describe the microanatomy of osseous tissue
- List bones and bone regions where compact, trabecular, and diploe osseous tissue is found
Generally speaking, there are two different types of osseous tissue; compact and spongy. The various bone organs of the skeletal system have different proportions of both of these types of bone tissues depending on their functions.
is typically found in areas where there is a significant stress on the bone, usually in one particular direction. This is especially evident in the shaft of s. Compact bone is very dense and resilient and is comparable to concrete in terms of compressive strength. Cement blocks are designed to withstand an incredible amount of compression such as supporting the weight of a house. Similarly, long bones support the weight of your body and are thickest in areas that are more weight-bearing and therefore experience the most compression. For example, the tibia (the weight-bearing bone of the lower leg), has a tremendous amount of compression along the longitudinal axis. It is in this area of the tibia where compression is greatest and thus the compact bone is thickest.
Both concrete and compact bone have impressive compression strength, but concrete has little if any tensile strength (resisting being pulled apart). This is why weight-bearing concrete should be reinforced with a rebar (steel bars embedded inside the concrete). The structure of reinforced concrete can be used as an analogy to understand the structure of compact bone. Compact bone gets its compressive strength from calcium and phosphate crystals but its tensile strength comes from collagen fibers. These collagen fibers are analogous to the rebar in reinforced concrete. They provide a framework for the deposition of the calcium phosphate salts and impart a tremendous amount of tensile strength while maintaining some flexibility.
Although compact bone is a solid matrix, the living bone cells are interconnected and the blood supply allows for the continual exchange of nutrients and waste products. The Haversian system consists of fluid-filled passageways throughout the bone solid matrix linking the various bone cells to the blood supply. The large passageways containing blood vessels are called canals. These canals have different names depending on the location within the bone organ.

Fig 6.2: Diagram of Compact Bone
The basic functional unit of compact bone is called an (Haversian system) which is a structure produced by concentric cylinders of a bone ground matrix called concentric lamellae with bone cells dispersed in between the layers. In the middle of each osteon is a ; a passageway for blood delivery to each osteon. Branching from the central canal are (tiny canals) that connect to every bone cell within the osteon. Each bone cell sends slender processes through these canaliculi linking them to each other and the blood vessels in the central canal. Larger perforating (Volkmann’s) canals connect the blood vessels of the central canal to the larger blood vessels outside of the bone.
Trabecular or spongy bone: While the outer portion of all bones are made of compact bone, the inner portions contain either spongy bone or a medullary cavity. Spongy bone is different from a compact bone in that it does not contain osteons. Instead, it contains small struts or slivers of bone called (“cross beam”). These little struts of bone branch out, creating a three-dimensional framework that appears, up close, to look like a sponge. Because spongy bone is sandwiched in between the compact bone layers it is formed where compressive stresses are lower. Because of the spaces between the slivers of osseous tissue, spongy bone is much lighter than compact bone but still provides a great deal of resistance against compression and in many different directions. The spaces between the trabeculae are called and contain bone marrow.
6.3 Connective Tissues of Bone
![]() 6.3 Learning Outcomes
6.3 Learning Outcomes
- Distinguish between ligaments, tendons, , and the periosteum
- List the roles of collagen in imparting strength and dissipating energy due to mechanical stress
Bone Connections and Collagen
Ligaments link one bone to another bone, whereas tendons tie (anchor) muscles to bone. These attachments between bone and tendons and ligaments are some of the strongest in the human body. However, these connective tissue attachments can be subjected to tremendous strain. Bones are surrounded by a fibrous capsule called the . The collagen fibers of the periosteum are continuous with the collagen fibers of the tendons and ligaments and even extend deep into the bone matrix to anchor them. Collagen fibers deep within the bone also help to alleviate mechanical stress. Sacrificial bonds between the collagen fibers assist in dissipating energy caused by mechanical stress. These bonds can break and reform, allowing bone to absorb stress without fracturing or breaking.
Bone Cartilage
There are places along the skeleton where bones join with . A point where bones come together is known as . As discussed in the tissue chapter, the most abundant type of cartilage is known as hyaline. This cartilage serves as a critical component involving bone growth and is also found in between bones where they meet with one another at various joints. Fibrocartilage, named for its dense parallel collagen fiber configuration, is found at “symphysis” joints. These joints are found in between vertebrae, pubic bones, and other joints that are subjected to great force. Fibrocartilage is an ideal tissue due to its ability to resist compression between bones.
6.4 Shape Classifications of Bones
![]() 6.4 Learning Outcomes
6.4 Learning Outcomes
- List the 6 types of bone shapes
- Name one bone for each shape classification

Fig. 6.3: Classifications of Bones
The bones of the human body can be classified into 6 general categories based on their shape as follows:
Long bones: As the name implies, long bones are long and slender. They make up the majority of bone mass in the upper and lower extremities of the body. For example, long bones of the upper extremities consist of the humerus, radius, and ulna. The femur, tibia, and fibula are the long bones making up the lower extremities. Not all long bones are as long as these. For example, the finger and toe bones are also considered long. Some of the long skinny bones of the skeleton have a different microanatomy and are therefore not considered long bones. For instance, ribs are considered s due to the internal tissue structure. Long bone microanatomy shows a thick layer of compact bone, especially in the long shaft or diaphyseal region. Inside of the compact bone is spongy bone tissue and, in the shaft, a medullary cavity that may contain red or .
s: Short bones are found primarily in the carpal (wrist) and tarsal (ankle) regions of the body. These are box-like, short, and stout bones that are more or less equal in width and length. These bones lack s or s. Some texts include the s in this category.
Flat bones: Most skull bones are flat bones. Flat bones can also be found in other regions of the skeleton including the ribs, sternum, and scapula (shoulder blade). Flat bones, as their name implies, are flat and have a thin layer of spongy bone sandwiched between the outer compact bone.
s: Irregular bones take on various complex shapes, are neither flat nor long, and have multiple projections. A good example of an irregular bone is a vertebral bone.
Sesamoid bones: These bones typically develop within a tendon and are the result of compression. The best example of a sesamoid bone is the patella, or knee cap, which develops during the period that an infant/young toddler crawls on its knees. It should be noted that sesamoid bones can develop in other areas of the body subjected to constant compression such as in the inner thigh of a Paniolo (Hawaiian cowboy), as a result of constantly riding horses.
Sutural (Wormian) bones: These bones are highly variable from individual to individual. They typically develop along the sutures or connections between the flat bones of the skull. They typically range in size from the tip of a pen to silver dollar size. Individuals may have none or many of these.
6.5 Long Bone Anatomy
![]() 6.5 Learning Outcomes
6.5 Learning Outcomes
- Describe the basic anatomy of a long bone
- Distinguish between the epiphysis, metaphysis, and diaphysis
- Describe the location of articular cartilage, periosteum, and endosteum
- Describe the vascularization and innervation of bone

Fig. 6.4: Anatomy of a Long Bone
As described above, long bones make up the bulk of the bone mass and length of the upper and lower extremities. The long bones of the upper extremities consist of the humerus of the arm which articulates with the two long bones of the forearm called the radius and ulna. The long bones of the lower extremities consist of the femur of the thigh articulating distally with the long bones of the lower leg called the tibia and fibula. Appreciate the similarities between the bones of the upper versus the lower extremities. Note that both the upper and lower extremities consist of one proximal bone articulating with two distal bones.
Each long bone has enlarged ends called the proximal and distal connected by a long shaft called a via a metaphysis. [see Figure 6.4]. You will notice from the image that the inner portions of the proximal and distal epiphysis contain spongy bone. Recall that spongy bone is present in areas of bone that endure stresses from many different directions. This is especially important in the epiphyses since they form moveable joints that compress from multiple directions and are the attachment points for many ligaments and tendons that pull from many directions.
In growing long bones, the or growth plate is a region composed of hyaline cartilage. As described later in this chapter, the epiphyseal plate is an area of the long bone that allows the bone to grow longer from its distal and proximal ends. This growth, known as interstitial growth, occurs through the process of endochondral which is the growth of cartilage that is then replaced with bone. When we stop growing in height as young adults, the cartilage of the epiphyseal plate is completely replaced by bone, leaving a visible line called the .
The metaphysis is the region between the epiphysis and diaphysis in which the chondroblasts of the epiphyseal cartilage are rapidly dividing, enlarging, and dying in the process of endochondral ossification.
The diaphysis is the “shaft” of the long bone and contains an outer ring of compact bone and an inner medullary cavity. Investigation of the compact bone of the diaphysis will show that it is constructed of thousands of osteons that run parallel to the long axis of the bone and extend the length of the diaphysis. The osteons add to the compressive strength of the bone while still allowing an extensive blood supply to access the different regions. Within the center of the diaphysis is found a hollow space called the medullary cavity in which we find bone marrow. At birth, this is all involved in erythropoiesis, but as a person ages, the red marrow of the medullary cavities is replaced by adipose tissue to become yellow marrow. In later adulthood, red marrow is found in the central or axial bones such as the vertebrae and also in the hip bones and the proximal epiphysis of the femur and humerus.
![]() Retrieval Practice
Retrieval Practice
Study the previous section about long bones, including every detail of the long bone figure. Put away the book and your notes. Create a sketch of the long bone, including all the labels you can recall from the figure. Get up and move around a little bit, giving your mind and eyes a brief break, and then take another look at your sketch. Is there anything you can add at this point? Once you have everything down you can remember, go back to the book and make corrections and additions based on the long bone figure.
Linings and Membranes of Bone

Fig. 6.5: Periosteum and Endosteum
The periosteum is a membrane that has an outer portion composed primarily of dense irregular connective tissue. This membrane serves as a layering around the bone that provides a passageway for blood vessels, lymphatics, and nerves. The joint capsule of synovial joints that merge articulating bones is a continuation of this periosteum. In addition to providing a tough outer layer for bones, collagenous (rope-like) fibers of the periosteum are continuous with the collagen fibers of the bone matrix itself and are called perforating (Sharpey’s) fibers. As stated earlier, the outer fibrous layer contains numerous collagen fibers that give the periosteum a tough resilient covering surrounding each bone. In addition, the periosteum has an inner osteogenic layer that contains cells playing a role in bone growth and repair. In addition to their connection with bones and joint capsules, collagen fibers of the outer periosteum intertwine with the collagen fibers of tendons and ligaments. This intertwining provides an incredibly strong attachment between bone, muscle, tendon and ligaments, and joint capsules.
The is an incomplete (not always present) cellular layer lining the inner medullary cavity, the central canals, and the trabeculae of spongy bone. The endosteum is similar to the osteogenic layer of the periosteum.
![]() Clinical Application
Clinical Application
You work as a Medical Forensic Specialist. You were called to visit the Kaumana Cave and found different bones. You have many questions. Are they human? If so, was the person male or female? How old was the person at death? How tall was the person? How long has the person been dead? What was the most probable cause of death? The forensic anthropologist is best suited to recover and investigate these remains and provide answers to these questions. For instance, to determine the age of death, one relevant anatomical information you will need is to determine whether the skeleton shows separate epiphyses and diaphyses or if these parts are fused together. If they are fused together, then the remains probably belong to a young person, and not an adult. Sex can be determined by visual inspection, followed by specific measurements. For instance, the female pelvis is designed to offer optimal space for the birth canal, which is reflected in its anatomy. Sex can also be investigated by analyzing the skull. Female skulls are smoother than male skulls, which are larger, with more pronounced areas for muscle attachment and squared mandible. One method to estimate how tall a person was, is to measure the height of the skull, the spine, and the lengths of leg bones and compare them with standard measurements. If you want to know more: From the Anthropology Department, Clark College, Vancouver, Wash, and the Medical Examiner Division, Oregon Department of State Police, Portland, Ore. Reprint requests to Dr. Lundy, Clark College, 1800 E McLoughlin Blvd, Vancouver, WA 98663; or e-mail: jlundy@clark.edu
Blood and Nerve Supply of Bone
Bone is a highly vascular tissue. As stated earlier, the solid matrix of bone has a series of tunnels and canals that allows blood and nutrient supply to each individual cell in the bone matrix. The marrow cavities are especially vascular. The fastest way to get fluids into a patient is through intraosseous (i.o.) infusion. In battlefield or emergency medicine, a device can quickly be stabbed into the sternum to give life-saving fluids. In addition to its rich blood supply, bone contains a dense network of nerve fibers. In other words, bone is innervated. The periosteum of bone is infused with nociceptors (pain receptors) that will signal the CNS in the case that there is tissue damage (an injured portion of bone). One example of the nociceptors of the periosteum is a sternal rub. This highly painful procedure is done to assess a patient’s ability to respond to pain when determining their Glasgow coma scale score.
6.6 Bone Cells
![]() 6.6 Learning Outcomes
6.6 Learning Outcomes
- List the various types of osteocytes
- Describe how these cells live in the hardened bone matrix
- Describe how these cells coordinate to maintain the bone matrix

Fig. 6.6: Bone Cells
Bone contains four types of cells. Osteoprogenitor cells, s, s, and s.
Osteoprogenitor cells (s) can be found as a component of both the periosteum and endosteum. They are involved with the repair of injury and the production of new bone cells as they can still divide and differentiate into osteoblasts.
Osteoblasts are active matrix-producing cells. As stated earlier, cells with blast in their suffix refer to cells that are actively secreting matrix. As osteoblasts secrete bone matrix, before the salts are deposited, the matrix is referred to as . Osteoblasts also stimulate the deposition of calcium phosphate crystals or hydroxyapatite to form mature bones.
An osteoblast becomes an osteocyte once it has surrounded itself with a bone matrix and becomes enclosed within a space known as a lacuna. Osteocytes are less active but are important in maintaining the bone around them and monitoring stress and initiating . Recall that although the bone matrix is solid, each individual osteocyte is provided with a blood supply by way of cytoplasmic extensions that permeate throughout the tiny, microscopic spaces in the bone matrix known as canaliculi (little canals) [see figure 6.7]. These canaliculi connect the blood vessels of the central and s to surrounding cells.

Fig. 6.7: Spongy Bone
Osteoclasts are giant multinucleated cells that are not related to osteogenic cells, instead, they are derived from the stem cells that produce monocytes and macrophage white blood cells. These cells secrete digestive enzymes and pump out hydrochloric acid that breaks down the collagen and minerals of the bone matrix. They can be thought of as having an opposite function to osteoblasts. While osteoblasts build up the bone matrix, osteoclasts meander through the bone matrix (like a worm tunneling through an apple), devouring and breaking down the bone matrix as they go.
Osteoblasts and osteoclasts play an important role in both the maintenance and destruction of the bone matrix. Their activity level is influenced by hormones involved with the maintenance of homeostatic levels of blood calcium discussed later in this chapter. Although we think of bone as solid and unchanging, bone is a living and dynamic tissue with cells that respond to changes in the environment. This causes the bone to be in a constant state of remodeling. In other words, osteoclasts are continually breaking down the bone matrix and osteoblasts are constantly building up in response to hormones and physical forces monitored by osteocytes. Typically, in adolescence when a person is growing and adding bone mass, the activity level of osteoblasts exceeds the activity of osteoclasts. Thus bone mass is added to the overall skeleton. In later years, the opposite may be true. As a person ages, osteoclast activity may exceed osteoblast activity, and overall, bone mass declines. Many physical and environmental factors play a role in the overall bone mass of an individual, including activity level and diet. This will be discussed later in the chapter.
6.7 Bone Matrix
![]() 6.7 Outcomes
6.7 Outcomes
- Explain how collagen contributes to the physical properties of bone tissue
- Describe the role of calcium in the ground substance of the bone matrix, and list some of the functions of calcium in your body outside of bone tissue.
- Describe the roles of vitamin C and vitamin D in the formation of bone matrix
![]() Cultural Connection
Cultural Connection
In Hawai’i, makau (fish hooks) have often been made from bone and used as traditional tools for gathering food. In ancient Hawai’i, the livelihood of kanaka was dependent on resources from the sea, so makau needed to be strong and resilient to last for many uses. The strength and integrity associated with the ground matrix of bone allows for the makau to support the weight of large fish and sharks. Makau are also made to signify great strength and prosperity and are often highly regarded for these characteristics. Such items have been passed from generation to generation and are highly prized. In Polynesian mythology, the god Māui is said to have used a hook made from the jawbone of his grandmother, Murirangawhenua, not only to catch great fish but also to ensnare the sun. Modern makau often seen in stores for purchase are typically carved from cow or whalebone.

For more examples, see: Bishop Museum image of makau: http://data.bishopmuseum.org/ethnologydb/type.php?type=fishhook and image of Murirangawhenua offering her jaw bone: https://teara.govt.nz/en/artwork/28358/muriranga-whenua
Recall that approximately one-third of the bone matrix is organic collagen fibers. This provides bone with its tensile strength, allowing bones to bend and flex to a great extent without breaking. Calcium phosphate crystals that make up hydroxyapatite make up the other two-thirds of bone mass.
 |
 |
| Hydroxyapatite in cattle bones | Hydroxyapatite in oxtail soup |
Fig. 6.8: Hydroxyapatite in cattle bones and oxtail soup
As mentioned at the beginning of the chapter, bone functions as an important reservoir for calcium and phosphate. In addition to providing bone compressive strength, the calcium of hydroxyapatite is a critical component required for proper skeletal and cardiac muscle physiology, cellular exocytosis, and blood clotting. Therefore, it is critically important to keep blood calcium levels maintained within a very narrow concentration range because hypocalcemia (low blood calcium) or (high blood calcium) can be fatal. As discussed later in the chapter, it is also important for bones to have enough mineral salts to prevent them from becoming soft and fragile.
Deposition of calcium into the bone or removal of calcium from bone is controlled by osteoblasts and osteoclasts responding to hormones such as parathyroid hormone and calcitonin. Vitamin D also assists calcium deposit as well as increasing calcium absorption from the gastrointestinal tract. The pathway to vitamin D production and activation begins with a cholesterol derivative in the skin being converted to cholecalciferol (Vitamin D3) via UV radiation. Vitamin D3 is a commonly added nutrient due to its important role in bones and calcium homeostasis. Cholecalciferol is then converted to calcidiol in the liver by the addition of a hydroxyl group and then to the final active form calcitriol in the kidneys by the addition of a second hydroxyl group.
Like vitamin D, vitamin C is another important molecule for strong healthy bones. Among other things, vitamin C is a cofactor in collagen protein production. Remember collagen is a fibrous (rope-like) protein in the bone matrix. A deficiency in vitamin C prevents covalent cross-linking of collagen fibrils, resulting in the disease known as scurvy. Due to the compromised bone matrix, scurvy patients have symptoms such as bleeding from the gums. Because of the lack of vitamin C-rich citrus fruit on long sea voyages, sailors used to be seen sucking on limes to prevent scurvy, leading to the nickname of “limeys”.
The traditional Hawaiian diet has a high fiber and mineral content. For example, kalo (taro) leaves used in laulau and ʻulu are rich in vitamin C and calcium. Did you know that vitamin D deficiency leads to not only a drop in bone density but also affects your immune health? A healthy immune system is important to keep the body in balance and fight cancers. Foods such as fatty fish, fish oils (think lomi lomi salmon), and liver are all rich in vitamin D. Most people in the United States consume less than the daily recommended vitamin D intake, and the vitamin D deficiency rate jumps to even higher among people with darker skin tone because the skin pigment blocks sunlight absorption necessary for vitamin D production. Diets low in vitamin D are more common in people who have a milk allergy or lactose intolerance, and those who consume a vegan diet.
6.8 Bone Growth
![]() 6.8 Learning Outcomes
6.8 Learning Outcomes
- Explain how intramembranous ossification forms bone tissue from mesenchymal tissue
- Explain how endochondral ossification forms bone tissue from a hyaline cartilage frame
- Contrast bone formation via intramembranous ossification with
- Explain major cell and tissue events that occur in interstitial growth and appositional growth
- Compare interstitial growth and appositional growth and how they change the shape of a bone
- Locate where epiphyseal plates are, explain their role in interstitial growth, and describe changes in the epiphyseal plates as a person ages
- Name hormones that affect bone growth and describe their effects on growth
- Name hormones that affect calcium content in bone tissue and explain how those hormones maintain calcium homeostasis between bone tissue and the body.
Cartilage growth can occur within the middle of bone tissue or along the outside edge of its width. When growth occurs inside or within bone tissue, it is called interstitial growth (“inter-” = between, “interstitial” = between the tissues). Whereas growth along the circumference of a bone is called appositional growth. Appositional growth begins with stem cells located within the . As those stem cells undergo mitosis and divide, they produce chondroblasts. The matrix secreted by the chondroblasts is eventually replaced by a bone matrix, thus thickening the circumference of the original bone. Interstitial growth occurs when chondroblasts divide and secrete cartilage matrix near the ends of a long bone. As the chondroblasts create more cartilage, the cartilage is eventually replaced by new bone tissue, thus lengthening the original bone. During the early stages of development, both appositional and interstitial growth occur simultaneously, however as cartilage matures, interstitial growth slows significantly and eventually stops. In adults, cartilage growth only occurs after an injury, and usually quite slowly due to the minimal vascularization of cartilage tissue.

Fig. 6.9: Longitudinal Bone Growth
 |
|
| 6.10.a: Interstitial Bone Growth | |
 |
|
| 6.10.b: Interstitial Bone Growth Detail | |
 |
|
| 6.10.c Interstitial and Appositional Bone Growth | |
 |
|
| 6.10.d: Appositional Bone Growth |
Fig. 6.10: Appositional vs interstitial growth
Bone growth is called ossification or osteogenesis (the generation of bone). Similar to cartilage, ossification can also occur deep within a tissue (interstitial) or along the outside edges of a tissue (appositional). All the various bone shapes can be generated through either one of two distinct processes of bone organ development. generates flat and some irregular bones of the skull, while endochondral ossification generates most of the bones of the skeleton, including all long bones.
Intramembranous Ossification
Intramembranous ossification (“intra-” = within, “membrane” = flat, sheet-like structure, “oss-” = bone) begins when s emerge from a thickened layer of embryonic mesenchyme. These early multipotent cells differentiate into osteoprogenitor cells and then osteoblasts. Osteoblasts secrete a matrix called osteoid, which hardens as calcium is deposited and crystallizes within the matrix. The osteoblasts eventually become trapped within pockets of bone matrix called . Once an osteoblast is contained within lacunae, they mature into an osteocyte. The initial bone tissue is poorly and randomly organized around blood vessels woven throughout the membrane, resulting in sponge-like structures called trabeculae within the inner regions of these bones. The periosteum covers the surface of bones formed through intramembranous ossification and also covers an underlying layer of osteoblasts. As bone remodeling takes place, the osteoblasts underneath them form lamellar (plate-like) compact bone tissue that protects the outer surfaces, while the inner portion remains spongy. The porous inner layer of flat bones is called diploe.
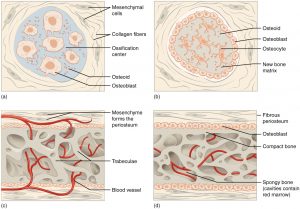
Fig. 6.11: Intramembranous Ossification
Endochondral Ossification
Endochondral ossification (“endo” = within, “chondral” = cartilage) begins with a hyaline cartilage frame that is gradually replaced by osseous tissue. The first step in this process is when osteoblasts form s within cartilage and secrete a ground matrix that accumulates calcium. This process of accumulating calcium within tissues is called calcification. As the matrix surrounding chondrocytes starts to calcify, the chondrocytes die, leaving empty lacunae (cavities). As these lacunae form, new blood vessels form around and penetrate the developing bone tissue through the process of angiogenesis (blood vessel formation). The new blood supply carries nutrients and oxygen needed to feed bone cells and create a new matrix. Osteoblasts will move into the cartilage and start producing osteoid, making little slivers of bone known as trabeculae, which are shaped based on the distribution of lacunae left behind by chondrocytes. The bone grows in both directions from the periosteal bud; a passageway of blood vessels that runs from the periosteum to the bone shaft. The first area where the previous steps occur is the primary ossification center, as it is the first site in the cartilage to form bone tissue. After the primary ossification center has formed, s emerge within both the proximal and distal epiphysis. These new ossification centers are formed by new blood vessels that also bring in osteoblasts to these sites, thus starting calcification of hyaline in more locations in the original cartilage scaffold. Eventually, all the hyaline will be replaced by bone matrix, except for articular hyaline that covers the very ends of a long bone, and the epiphyseal plate located between the epiphysis and diaphysis of a long bone.
Throughout childhood, the epiphyseal plates are present as the mitosis of chondrocytes and the formation of new hyaline cartilage in the epiphyseal plates keeps pace with the production of bone that replaces the cartilage. As you age into adulthood, your formation of bone within the epiphyseal plates outpaces the mitosis of the chondrocytes, and the epiphyseal plate eventually becomes solid bone. The bony site where the last remnants of the epiphyseal plate are found is known as the epiphyseal line. Long bones reach full maturity and length between 10-25 years of age (depending on the bone and sex), and once there is no more cartilage in the epiphyseal plate, a long bone can grow no longer. Typically, the epiphyseal plates of long bones fuse at around age 13-15 for females and 15-17 for males. However, other bones, such as the hip bones, may fuse later in life around the age of 25.

Fig.6.12: Endochondral Ossification
Within each epiphyseal plate, there are five zones at different stages of bone growth and ossification. The resting zone is nearest to the epiphysis and appears as regular hyaline cartilage. This resting zone merely anchors the epiphysis to the diaphysis. Adjacent to this zone is the proliferating zone, where chondrocytes are undergoing mitosis at a high rate. The chondrocytes divide so rapidly, that instead of pushing away from each other as in normal cartilage, the cells stack on top of one another, producing long column-shaped lacunae. The next layer is the hypertrophic layer (“hyper” = excessive, “trophy” = growth) in which the chondrocytes stop dividing, but are increasing in size. This causes the cartilage walls between adjacent lacunae to thin and break down. Eventually, minerals start to accumulate in the matrix and destroy the chondrocytes. The area where this initial deposit of calcium and minerals occurs is called the calcified zone, and the process of depositing calcium and minerals is called calcification. Ossification is the organized hardening of bone by osteoblast activity and occurs in the ossification zone. Most changes in bone length occur in the proliferation and hypertrophic zones, but the final ossification zone makes the new tissue matrix strong and resilient.

Fig. 6.13: Progression from Epiphyseal Plate to Epiphyseal Line As a bone matures, the epiphyseal plate progresses to an epiphyseal line. (a) Epiphyseal plates are visible in a growing bone. (b) Epiphyseal lines are the remnants of epiphyseal plates in a mature bone.
The ends of long bones have localized areas called epiphyseal plates, which are sites of chondrocyte proliferation and cartilage matrix secretion, followed by replacement by osteoblasts and osteocytes. The formation of new bone tissue at the end of long bones is responsible for how your bones lengthen and cause you to grow in height. Since juveniles are still growing, their bones will have a clear epiphyseal plate of chondrocytes and cartilage, but adults who have stopped growing will lack epiphyseal plates and have their epiphysis fully fused to the diaphysis. Forensic anthropologists can look at the extent of union (epiphyseal plate ossification) to help determine the age of a bone. Epiphyseal plates in females unionize earlier than in males. The thickness of bones can also be informative about an individual’s age or physical activity (weight lifters have thick compact bone layers). Wolff’s law describes how the shape and microstructure of bone tissue are strengthened in proportion to the mechanical stress placed upon it.
 |
 |
| Young – open and partial open | Complete union, adult |
Fig. 6.14: x-ray showing different ages of epiphyseal lines.
Hormones Affecting Bone Growth
Much of the body’s physiology is regulated by hormones, which are molecules released by cells into the blood and which eventually bind receptors and cause changes to cells in another area of the body. The hormone most people think about when they think of body growth is growth hormone (GH; hGH in humans). [Study Tip: You will have to get used to memorizing acronyms when it comes to hormones.] Growth hormones are not the most powerful stimulators of bone growth, but they stimulate mitosis of chondroblasts within the epiphyseal plates, which gives osteoblasts more matrix to calcify and lengthen bones. Additionally, GH stimulates the release of insulin-like growth factors (IGFs) from the liver. Some IGFs are very potent stimulators of bone growth, and increased IGF concentrations in the body lead to increased bone mass.
Sex hormones (estrogens and androgens) increase chondroblast and osteoblast activity, causing rapid growth during puberty. However, osteoblast activity occurs at a higher rate in response to these hormones, and thus the rate of ossification overtakes the rate of producing hyaline cartilage at the epiphyseal plates. When the last bit of cartilage is finally ossified, this causes cessation of growth. Therefore the sex hormones are responsible for both the rapid growth experienced during your teenage years and the stoppage of growth that occurs in early adulthood.
Thyroid hormones increase the metabolic rate of most cells and a lack of thyroid hormone can result in delayed or reduced bone growth and mineralization, but the exact mechanism is unknown. Bone growth cannot occur without calcium or the other chemical building blocks of the ground matrix. Calcitonin helps build a new bone matrix by putting calcium “in” your bones. Calcitonin is released from specialized “C” cells (parafollicular cells) in the thyroid gland that work independently from the thyroid hormone-producing cells. Calcitonin targets osteoclasts and slows down their rate of bone resorption. The overall effect of calcitonin is to increase bone mass and decrease blood calcium levels as osteoclasts are not enzymatically breaking as much bone matrix and releasing the dissolved calcium ions into the blood.
Parathyroid hormone (PTH) is made by the parathyroid glands, which are little islands of cells that are located behind the thyroid gland. PTH does the opposite of calcitonin and takes calcium out of your bone tissue by increasing osteoclast activity. You may be wondering why would your body want to remove calcium from your bones? The reason is that calcium has many functions in your body besides being part of the bone matrix. Calcium is also necessary for blood clotting, cellular exocytosis, muscle contraction, and electrical activity in your brain; all of which are critical for life. If your dietary intake of calcium is inadequate or if your body has trouble absorbing calcium, your blood calcium levels will be low. If your blood calcium concentration is low, your body will try to increase your blood calcium to maintain calcium homeostasis and keep those previously mentioned vital functions running. Your body can increase the concentration of blood calcium ions by using the bone matrix as a calcium storage depot or “bank”.
In a healthy person, PTH and calcitonin are regulatory hormones that act to keep the blood calcium within normal homeostatic levels. When your blood calcium levels get too high, calcitonin will be secreted and your body can deposit excess blood calcium into your bone matrix. When your blood calcium levels get too low, your body can secrete PTH to release calcium from your bones and into your bloodstream.
Glucocorticoids (including cortisol in humans) are powerful hormones that regulate normal blood glucose levels, but cortisol is also known as “the stress hormone” because it increases during prolonged stressful situations or when normal sleeping patterns are disrupted. Excess cortisol levels in your body can depress growth within the epiphyseal plates. Serotonin helps to regulate normal bone remodeling but also has a deleterious effect on bone growth if there are excess serotonin levels in the body.
6.9 Bone Diseases and Injuries
![]() 6.9 Learning Outcomes
6.9 Learning Outcomes
- Describe how problems and pathologies affecting the bone matrix can result in bone diseases
- Explain how abnormal levels of hormones can affect bone growth and the role of hormones in bone diseases
- Describe how problems in cartilage and connective tissue can result in bone diseases and abnormal growth
- Explain how deficiencies in vitamins C or vitamin D can lead to poor bone health
- Describe the loss in bone density that occurs with age and how it relates to the risk of bone injury in elderly people
- Categorize and differentiate types of bone fractures
- Describe the process of how fractures heal
Developmental Diseases and Diseases Affecting Bone Growth
Osteitis deformans (Paget’s disease) is a disease that causes deformed osseous tissue as a result of rapid reabsorption of bone matrix followed by rapid and hasty deposition of new bone matrix. The new bone is poorly organized and is therefore weak and can cause pain. The disruption of osteoclast and osteoblast homeostasis is usually isolated to just a few bones (most frequently, the skull, vertebrae, pelvis, femur, or tibia). Osteitis deformans have an unknown cause as of this writing, but scientists and doctors suspect that genetic risk factors or viruses could be potential causes.
Gigantism is a result of too much growth hormone in children, leading to overgrowth of the skeletal system. This growth hormone excess is usually due to a pituitary tumor that produces too much growth hormone. In gigantism, the abundance of growth hormone causes cartilage cells in the epiphyseal plates to proliferate at a rapid rate. The overabundance of cartilage cells causes an overproduction of cartilage matrix that can undergo endochondral ossification, causing long bones to grow longer and longer. The rapid growth usually leads to poor bone formation and compromised strength.
Achondroplasia (“a-”= without, “-chondro” = cartilage, “-plasia” = tissue growth), is a disease characterized by the abnormal conversion of hyaline cartilage to bone tissue. This occurs when chondrocytes abnormally stop replicating. This disrupts endochondral ossification and prematurely halts epiphyseal plate formation and interstitial growth. Achondroplastic dwarfism is a type of achondroplasia that leads to premature cessation of long bone interstitial growth, causing a short stature of long bones. However, flat bones that grow via intramembranous ossification are not affected by this condition, since cartilage is not necessary for intramembranous growth. Therefore, people with achondroplasia have stunted long bones but a relatively normal head and thorax size.
Osteomalacia is a condition of poor bone mineralization due to inadequate absorption or bioavailability of calcium, phosphate, and/or vitamin D. When osteomalacia occurs in children the condition is called rickets and is more severe than osteomalacia in adults. Scurvy is another disease that affects bone due to nutritional deficiency in vitamin C. Vitamin C is needed to produce collagen, a major component of the bone matrix.
As we age, our bone cells start to decrease their protein synthesis and secretion of bone matrix. This causes the mineral composition of bone to decrease with age and causes bones to become less dense. The loss of bone density increases bone brittleness and the risk of breaking bones (). Osteopenia (“osteo-”= bone, “penia” = poverty) is the normal age-related loss of bone, whereas if the bone loss is abnormally excessive it is called (“osteo-” = bone, “-poros” = porous, having many holes). Osteopenia slowly begins in people around the age of 40. During that change, osteoblasts decline their production of osteoid, but osteoclasts continue cutting into and dissolving bone matrix. The vertebrae and jawbones are most affected by osteopenia. Osteoporosis occurs when the reduced bone matrix mass begins to compromise normal bone physiology. Several risk factors increase your chances of developing osteoporosis, including: smoking and alcohol consumption, age, sex (women are affected more than men), genetic factors [Caucasians and Asians are most affected], and hormone imbalances (low vitamin D). The areas most affected by osteoporosis include the hip, wrist, and vertebrae. Treatments for osteoporosis include diet and exercise. Exercise causes mechanical stress to bones, which induces bone remodeling that improves the organization and strength of bone tissue.
![]() Deep Dive
Deep Dive
About 80% of people in the U.S. with osteoporosis are women. One in two women over the age of 50 will break a bone due to osteoporosis. Do you wonder why osteoporosis is more common in females than males? When a female stops menstruating, she enters menopause and the hormone changes decrease her bone density. If even for a moment you think osteoporosis may not be that big of a deal, consider this: 85% of people who break a hip die within the first year of the fracture. The good news is, osteoporosis can be prevented. Be sure you and your dear ones talk to your healthcare provider about lifestyle habits to increase bone health and screening for early detection of osteoporosis. Share the information. Let’s get educated about osteoporosis to help people prevent it!
Osteogenesis imperfecta (brittle bone disease) is a genetic disease usually caused by a mutation of a collagen gene. Symptoms include brittle bones, short stature, and teeth issues but may also include a blue tinge in the white part of the eyes, hearing loss, and breathing problems.
Fractures
Fractures are breaks in a bone due to stress or insult (injury). Fractures become more frequent with aging as bones lose density and become weaker, and maintaining your balance becomes more challenging. Stress fractures occur due to chronic, repetitive physical activity that deprives the tissue of sufficient healing time. For example, an untrained person who starts a rigorous and prolonged exercise program may be susceptible to stress fractures of the bones of the lower limb, especially the tibia (shin bone). Pathologic fractures are a result of bone disease, such as tumors that develop in bone tissue.
Fractures can be categorized based on how the bone breaks. If the bone is broken but is still under the skin (the bone does not poke through the skin) it is called a simple fracture. Compound fractures are when a bone piece has pierced the skin. If the fracture contains many small pieces it is a comminuted fracture. Greenstick fractures are a type of incomplete fracture (not broken all the way across) when the bone is bent but not broken on at least one side. Greenstick and epiphyseal plate fractures are more common in children since their bones are more flexible and still growing in length. Pott’s fractures are fractures of the ankle bones that are a result of physical injury.

Fig. 6.15: Types of Fractures Compare healthy bone with different types of fractures: (a) closed fracture, (b) open fracture, (c) transverse fracture, (d) spiral fracture, (e) comminuted fracture, (f) impacted fracture, (g) greenstick fracture, and (h) oblique fracture.
| Type of Fracture | Description |
| Transverse | Occurs straight across the long axis of the bone |
| Oblique | Occurs at an angle that is not 90 degrees |
| Spiral | Bone segments are pulled apart as a result of a twisting motion |
| Comminuted | Several breaks result in many small pieces between two large segments |
| Impacted | One fragment is driven into the other, usually as a result of compression |
| Greenstick | A partial fracture in which only one side of the bone is broken |
| Open (or compound) | A fracture in which at least one end of the broken bone tears through the skin; carries a high risk of infection |
| Closed (or simple) | A fracture in which the skin remains intact |
If a bone is broken, it will first be realigned before it can be immobilized. The process of realigning a fractured bone is called reduction. Reduction of fractures often requires surgery. In some cases, closed fractures of a limb bone can be reduced by a doctor after viewing an X-ray and palpating the affected area. Traction involves using a device to assist in the reduction process by pulling on part of the body. Once the fracture is aligned, then it can be immobilized with a cast during the first three stages of healing.
Fractures can take just a couple of months or much longer to heal, depending on the severity and type of fracture and the age of the patient. The bone tissue repair process occurs in four stages. For any tissue to heal, nutrients and building materials are needed which are supplied by the blood. Capillaries are broken during a bone fracture, and the blood leaking from these vessels forms the first stage of bone healing, a hematoma (a swelling of a body part or region due to blood accumulation). Then, fibroblasts produce collagen protein fibers to provide structural support for the damaged tissue and chondroblasts secrete matrix to form a dense regular connective tissue. Together, fibroblasts and chondroblasts form a fibrocartilaginous callus (a hardened but flexible tissue). Over time, osteoblasts replace the fibrocartilage with trabecular bone, thus producing a bony callus. For the bone to become strong and resilient, remodeling must occur. In this phase, osteoclasts remove excess material, spongy bone is replaced with compact bone, and osteons become more organized. Therefore, it is important in the healing process for the bone to be subjected to mechanical stress (such as exercise) promptly so that these processes continue to be stimulated and remodel the damaged bone tissue.

Fig. 6.16: Bone healing four stages

Chapter Summary

Key terms
articular cartilage
thin layer of cartilage covering an epiphysis; reduces friction and acts as a shock absorber
articulation
where two bone surfaces meet
bone
hard, dense connective tissue that forms the structural elements of the skeleton
canaliculi
(singular = canaliculus) channels within the bone matrix that house one of an osteocyte’s many cytoplasmic extensions that it uses to communicate and receive nutrients
cartilage
semi-rigid connective tissue found on the skeleton in areas where flexibility and smooth surfaces support movement
central canal
longitudinal channel in the center of each osteon; contains blood vessels, nerves, and lymphatic vessels; also known as the Haversian canal
compact bone
dense osseous tissue that can withstand compressive forces
diaphysis
tubular shaft that runs between the proximal and distal ends of a long bone
diploë
layer of spongy bone, that is sandwiched between two the layers of compact bone found in flat bones
endochondral ossification
process in which bone forms by replacing hyaline cartilage
endosteum
delicate membranous lining of a bone’s medullary cavity
epiphyseal line
completely ossified remnant of the epiphyseal plate
epiphyseal plate
(also, growth plate) sheet of hyaline cartilage in the metaphysis of an immature bone; replaced by bone tissue as the organ grows in length
epiphysis
wide section at each end of a long bone; filled with spongy bone and red marrow
flat bone
thin and curved bone; serves as a point of attachment for muscles and protects internal organs
fracture
broken bone
hematopoiesis
production of blood cells, which occurs in the red marrow of the bones
hole
opening or depression in a bone
hypercalcemia
condition characterized by abnormally high levels of calcium
hypocalcemia
condition characterized by abnormally low levels of calcium
intramembranous ossification
process by which bone forms directly from mesenchymal tissue
irregular bone
bone of complex shape; protects internal organs from compressive forces
lacunae
(singular = lacuna) spaces in a bone that house an osteocyte
long bone
cylinder-shaped bone that is longer than it is wide; functions as a lever
modeling
process, during bone growth, by which bone is resorbed on one surface of a bone and deposited on another
open reduction
surgical exposure of a bone to reset a fracture
osseous tissue
bone tissue; a hard, dense connective tissue that forms the structural elements of the skeleton
ossification
(also, osteogenesis) bone formation
ossification center
cluster of osteoblasts found in the early stages of intramembranous ossification
osteoblast
cell responsible for forming new bone
osteoclast
cell responsible for resorbing bone
osteocyte
primary cell in mature bone; responsible for maintaining the matrix
osteogenic cell
undifferentiated cell with high mitotic activity; the only bone cells that divide; they differentiate and develop into osteoblasts
osteoid
uncalcified bone matrix secreted by osteoblasts
osteon
(also, Haversian system) basic structural unit of compact bone; made of concentric layers of calcified matrix
osteoporosis
disease characterized by a decrease in bone mass; occurs when the rate of bone resorption exceeds the rate of bone formation, a common occurrence as the body ages
perforating canal
(also, Volkmann’s canal) channel that branches off from the central canal and houses vessels and nerves that extend to the periosteum and endosteum
perichondrium
membrane that covers cartilage
periosteum
fibrous membrane covering the outer surface of bone and continuous with ligaments
primary ossification center
region, deep in the periosteal collar, where bone development starts during endochondral ossification
projection
bone markings where part of the surface sticks out above the rest of the surface, where tendons and ligaments attach
red marrow
connective tissue in the interior cavity of a bone where hematopoiesis takes place
remodeling
process by which osteoclasts resorb old or damaged bone at the same time as and on the same surface where osteoblasts form new bone to replace that which is resorbed
secondary ossification center
region of bone development in the epiphyses
sesamoid bone
small, round bone embedded in a tendon; protects the tendon from compressive forces
short bone
cube-shaped bone that is approximately equal in length, width, and thickness; provides limited motion
skeletal system
organ system composed of bones and cartilage that provides for movement, support, and protection
spongy bone
(also, cancellous bone) trabeculated osseous tissue that supports shifts in weight distribution
trabeculae
(singular = trabecula) spikes or sections of the lattice-like matrix in spongy bone
yellow marrow
connective tissue in the interior cavity of a bone where fat is stored
Sources
http://data.bishopmuseum.org/ethnologydb/type.php?type=fishhook
https://www.communitymedical.org/about-us/news/vitamin-d-a-hidden-deficiency-in-women-of-color
Vitamin D and Covid: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7385774/
https://www.nature.com/articles/s41430-020-0558-y
https://www.cdc.gov/nutritionreport/99-02/pdf/nr_ch2b.pdf
https://www.cdc.gov/nutritionreport/pdf/Second-Nutrition-Report-Vitamin-D-Factsheet.pdf
https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#h5
https://pantheon.org/articles/m/muri-ranga-whenua.html
Ka’ai, Tania. (2005). Te Kauae Maro o Muri-ranga-whenua (The Jawbone of Muri-ranga-whenua). PORTAL Journal of Multidisciplinary International Studies. 2. 10.5130/portal.v2i2.92.
Media Attributions
- olelo_noeau
- Diagram of Compact Bone © Openstax is licensed under a CC BY (Attribution) license
- Classifications of Bones © Openstax is licensed under a CC BY (Attribution) license
- Anatomy Long Bone © Openstax is licensed under a CC BY (Attribution) license
- Periosteum Endosteum © Openstax is licensed under a CC BY (Attribution) license
- Bone Cells © Openstax is licensed under a CC BY (Attribution) license
- Diagram Spongy Bone © Openstax is licensed under a CC BY (Attribution) license
- Wiki Fish Hooks USFWS_Smuggling_operation_(27952325113) © USFWS is licensed under a CC BY (Attribution) license
- Wiki Cattle_bone_(7292654216) © MAURO CATEB from Brazil is licensed under a CC BY (Attribution) license
- Wiki Oxtail Soup Kkori-gomtang © 굿바이 조미료 is licensed under a CC BY (Attribution) license
- Longitudinal Bone Growth © Openstax is licensed under a CC BY (Attribution) license
- F3 Interstitial Bone Growth Intechopen © Rosy Setiawati and Paulus Rahardjo, IntechOpen is licensed under a CC BY (Attribution) license
- F7 Interstitial Bone Growth Intechopen © Rosy Setiawati and Paulus Rahardjo, IntechOpen is licensed under a CC BY (Attribution) license
- Interstitial and Appositional Bone Growth © Rosy Setiawati and Paulus Rahardjo, IntechOpen is licensed under a CC BY (Attribution) license
- Appositional Bone Growth © Rosy Setiawati and Paulus Rahardjo, IntechOpen is licensed under a CC BY (Attribution) license
- Intramembranous Ossification © Openstax is licensed under a CC BY (Attribution) license
- Endochondral Ossification © Openstax is licensed under a CC BY (Attribution) license
- Progression Ephyseal Plate Ephyseal Line © Openstax is licensed under a CC BY (Attribution) license
- Wiki The_human_body_and_health_-_an_elementary_text-book_of_essential_anatomy,_applied_physiology_and_practical_hygiene_for_schools_(1908)_(14772671062) © Internet Archive Book Images is licensed under a Public Domain license
- Epiphyseal Plate Hand_Altersbestimmung © eigen is licensed under a CC BY (Attribution) license
- Types of Fractures © Openstax is licensed under a CC BY (Attribution) license
- Wiki Bone Healing 613_Stages_of_Fracture_Repair © OpenStax College is licensed under a CC BY (Attribution) license
- Honu_‘Iwalani Clayton_CCBY_2022 10 30 © ‘Iwalani Clayton is licensed under a CC BY (Attribution) license
- divider_maile
Bone tissue; a hard, dense connective tissue that forms the structural elements of the skeleton.
Hard, dense connective tissue that forms the structural elements of the skeleton.
Organ system composed of bones and cartilage that provides for movement, support, and protection.
Production of blood cells, which occurs in the red marrow of the bones.
(Also, cancellous bone) trabeculated osseous tissue that supports shifts in weight distribution.
Dense osseous tissue that can withstand compressive forces.
Cylinder-shaped bone that is longer than it is wide; functions as a lever.
(Also, Haversian system) basic structural unit of compact bone; made of concentric layers of calcified matrix.
Longitudinal channel in the center of each osteon; contains blood vessels, nerves, and lymphatic vessels; also known as the Haversian canal.
(Singular = canaliculus) channels within the bone matrix that house one of an osteocyte’s many cytoplasmic extensions that it uses to communicate and receive nutrients.
(Singular = trabecula) spikes or sections of the lattice-like matrix in spongy bone.
Layer of spongy bone, that is sandwiched between two the layers of compact bone found in flat bones.
Thin layer of cartilage covering an epiphysis; reduces friction and acts as a shock absorber.
Fibrous membrane covering the outer surface of bone and continuous with ligaments.
Semi-rigid connective tissue found on the skeleton in areas where flexibility and smooth surfaces support movement.
Where two bone surfaces meet.
Thin and curved bone; serves as a point of attachment for muscles and protects internal organs.
Connective tissue in the interior cavity of a bone where fat is stored.
Cube-shaped bone that is approximately equal in length, width, and thickness; provides limited motion.
Bone markings where part of the surface sticks out above the rest of the surface, where tendons and ligaments attach.
Opening or depression in a bone.
Small, round bone embedded in a tendon; protects the tendon from compressive forces.
Bone of complex shape; protects internal organs from compressive forces.
Wide section at each end of a long bone; filled with spongy bone and red marrow.
Tubular shaft that runs between the proximal and distal ends of a long bone.
(Also, growth plate) sheet of hyaline cartilage in the metaphysis of an immature bone; replaced by bone tissue as the organ grows in length.
(Also, osteogenesis) bone formation.
Completely ossified remnant of the epiphyseal plate.
Connective tissue in the interior cavity of a bone where hematopoiesis takes place.
Delicate membranous lining of a bone’s medullary cavity.
Primary cell in mature bone; responsible for maintaining the matrix.
Cell responsible for forming new bone.
Cell responsible for resorbing bone.
Undifferentiated cell with high mitotic activity; the only bone cells that divide; they differentiate and develop into osteoblasts.
Uncalcified bone matrix secreted by osteoblasts.
Process by which osteoclasts resorb old or damaged bone at the same time as and on the same surface where osteoblasts form new bone to replace that which is resorbed.
(Also, Volkmann’s canal) channel that branches off from the central canal and houses vessels and nerves that extend to the periosteum and endosteum.
Condition characterized by abnormally high levels of calcium.
Process in which bone forms by replacing hyaline cartilage.
Membrane that covers cartilage.
Process by which bone forms directly from mesenchymal tissue.
Cluster of osteoblasts found in the early stages of intramembranous ossification.
(Singular = lacuna) spaces in a bone that house an osteocyte.
Region, deep in the periosteal collar, where bone development starts during endochondral ossification.
Process, during bone growth, by which bone is resorbed on one surface of a bone and deposited on another.
Region of bone development in the epiphyses.
Broken bone.
Disease characterized by a decrease in bone mass; occurs when the rate of bone resorption exceeds the rate of bone formation, a common occurrence as the body ages.
Surgical exposure of a bone to reset a fracture.
