Anatomy and Physiology
23 Digestive System
ʻAi no i ka ʻape he maneʻo no ko ka nuku.
He who eats ʻape is bound to have his mouth itch.
He who indulges in something harmful will surely reap the result.
ʻŌlelo Noʻeau, compiled by Mary Kawena Pukui, #82
Introduction
 |
 |
Figure 23.1: Plate Lunch & Haupia
![]() Chapter Learning Outcomes
Chapter Learning Outcomes
- List and describe the anatomy and arrangement of the organs and accessory organs of the digestive system
- Discuss the fundamental processes that regulate movement and digestion along the entire digestive tract
- Discuss the contribution and roles of the liver, pancreas, and gallbladder in digestion
- Compare and contrast the digestion of macronutrients across different organs of the digestive system
The billions of cells in your need various nutrients, water, and ions to sustain life and perform their functions. These critical components are provided by a functioning digestive system. The digestive system is involved with the mechanical and chemical breakdown (digestion) of nutrients. An important concept is that nutrients need to cross the epithelial lining of the digestive tract to be absorbed by the body. After nutrients are absorbed by the epithelium, they are transported to the rest of the body by entering the bloodstream or lymphatic system. Before this process can occur, these nutrients need to be broken down into essential components that are small enough to be transported across cell membranes.
For example, when you eat spam musubi, the complex carbohydrates in the rice need to be broken down into simple sugars, the proteins in the meat need to be broken down into individual amino acids, and the fats need to be emulsified and broken down into fatty acids and monoglycerides to cross the epithelial lining of the “gut” and into the bloodstream.
![]() Food and Environment
Food and Environment
Spam Musubi
An immensely popular snack and lunch food, and a potluck staple in Hawaiʻi i is Spam musubi; a slice of grilled Spam on top of (or sandwiched between) a block of rice, wrapped with nori (dried seaweed). Musubi is a Japanese word for a ball of rice wrapped with nori. SPAM is a canned lunch meat product created in Minnesota and first hit shelves in 1937. Toward the end of the Great Depression, it filled a huge need for inexpensive meat products. During World War II, due to its ability to be stored for long periods, it could be easily shipped around the world and it became a household staple. Today, SPAM products are available in 44 different countries and over eight billion SPAM products have been sold worldwide. There is even a SPAM museum in Minnesota, its birthplace! According to the manufacturer, SPAM only contains six ingredients — pork with ham meat added, salt, water, potato starch, sugar, and sodium nitrite.
The origin of Spam musubi is disputed but commonly considered to be during World War II when canned meat was incorporated into local cuisines wherever American troops were stationed. Now there are many variations of this local favorite; Spam musubi with egg, furikae, bacon, and many more. Now there are even cookbooks specifically for Hawaiian-style musubi. So, we should all be proud of our Hawaiian culinary inventiveness!

Figure 23.2: ʻOno SPAM Musubi
To accomplish the complicated process of breaking down foodstuffs into their basic components, the digestive system utilizes various organs along the digestive tract or gastrointestinal tract (GI tract, also ) and accessory organs. Although the GI tract is continuous, different portions of the GI tract vary considerably in function. These differences in function will be reflected in the various appearances and arrangements of the walls of the different portions of the GI tract. The physiological function of a particular region of the tract is reflected not only in the gross anatomy of the organ but also in the microanatomy.
![]() Cultural Connection
Cultural Connection
Naʻau and the Native Hawaiian concept of unification of the heart and mind — our “gut instinct”.
As is the case with many Hawaiian words, naʻau (“nah-ow”) has many meanings, depending upon which context it is used. It is often used to refer to the visceral organs of an animal or the mind; the heart; the seat of moral powers. Often naʻau is part of other compound words like naʻauao, which is often interpreted to mean “an enlightened mind” or “wisdom”. When taken in a broader context, naʻauao refers to the Hawaiian concept of the brain in your gut — what contemporary science re-discovered and calls the enteric nervous system. The enteric nervous system consists of millions of sensory and motor neurons embedded in the stomach, small intestine, and large intestine. Along with interneurons, these neural circuits connect your brain to your visceral organs, creating synapses that unite emotional responses with visceral functions. While the enteric nervous system sends sensory information and receives motor feedback from the CNS, it can also work autonomously, detecting changes to the visceral environment and independently stimulating localized responses. So, yes, your body has two brains — the one we are all familiar with within the skull, but also a vitally important one found in the gut. Ever wonder why you get “butterflies” in your stomach before a big date? Or why you feel nauseous before a big event? Or why you just know that something “feels wrong”? The answer lies within the complex communication that exists between the CNS and the enteric nervous system in the gut.
 |
 |
Figure 23.3: Poi and Laulau
23.1 Overview of Digestive System
![]() 23.1 Learning Outcomes
23.1 Learning Outcomes
- Identify the organs of the alimentary canal from proximal to distal, and briefly state their function
- Identify the s and briefly state their function
- Describe the four fundamental tissue layers of the alimentary canal
- Contrast the contributions of the enteric and autonomic nervous systems to digestive system functioning
- Explain how the peritoneum anchors the digestive organs
- Discuss the processes and control of ingestion, propulsion, mechanical digestion, chemical digestion, absorption, and defecation
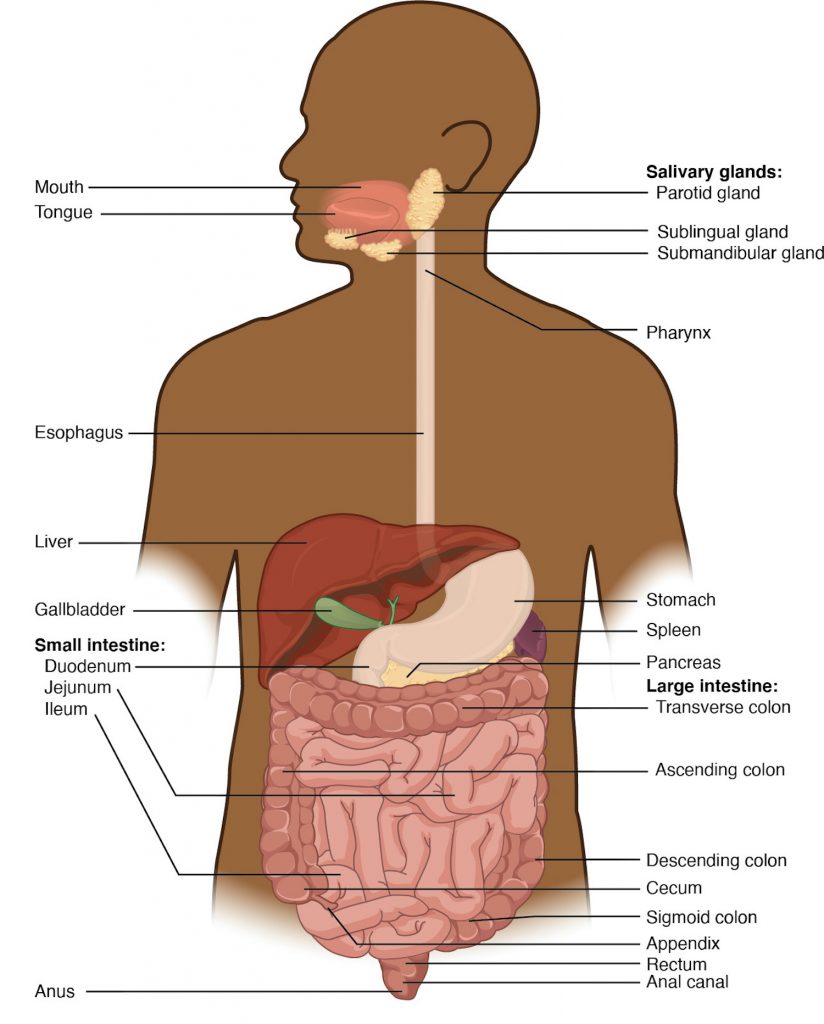
Figure 23.4 Components of the Digestive System from OpenStax
The GI tract extends from the mouth () to the anus. The majority of the entire GI tract consists of a muscular tube. This muscular tube will always display four distinct layers. They are arranged from deep to superficial: tunica , , , and /adventitia.
Although the four layers will always be present along the entire length of the GI tract, the anatomy of each of these layers changes based on the function.
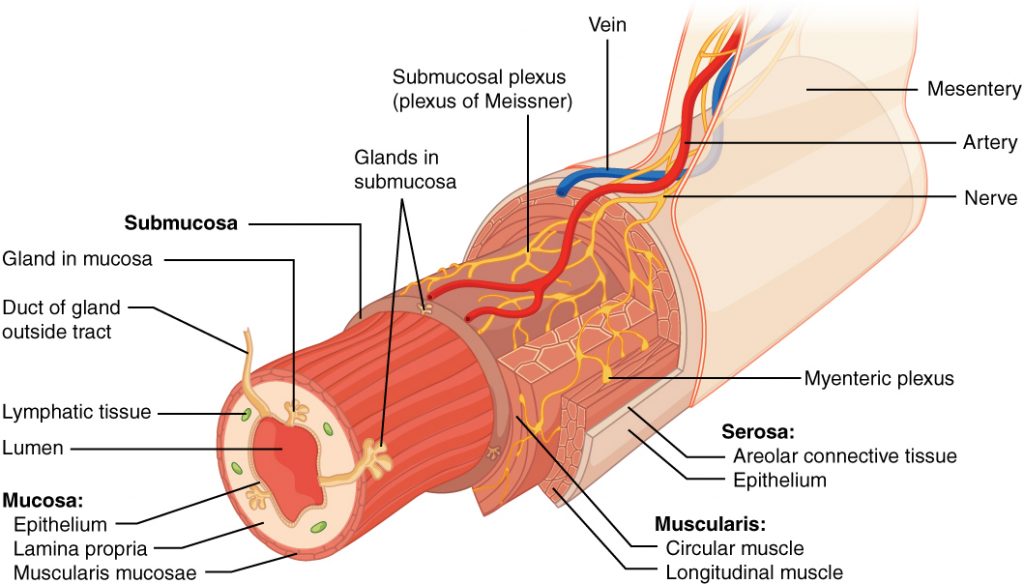
Figure 23.5 Layers of the Alimentary Canal from OpenStax
Overall histology of the digestive tract
The tunica mucosa is the innermost layer of the GI tract and consists mostly of a mucous membrane. The epithelium that lines this layer can be stratified or simple. Areas of the GI tract that are exposed to abrasion are lined with thicker stratified squamous epithelium, and areas that have mucous secretions consist of simple columnar epithelium. A memorization trick is to remember that the beginning and end of the GI tract are exposed to abrasion (ingested food at the beginning and fecal matter at the end). As a result, the mouth, , and are lined with stratified squamous epithelium as well as the anus, which is the very end of the GI tract. The portions of the GI tract located between the esophagus and anus are lined with a simple columnar epithelium. Simple columnar epithelium can be found in the , small and s, and the simple columnar cells in those organs are involved with more complicated functions such as excretion and , which will be discussed later in this chapter.
Just superficial to the columnar epithelium is a thin layer known as the lamina propria. This layer consists of areolar connective tissue. Recall from our tissue chapter [link to tissue chapter] that areolar tissue is an optimal tissue to provide scaffolding and routes for passage of blood and lymphatic vessels (for purposes of absorption and gas exchange), and serves as a route for nerve passage. In addition, the mucosa layer contains a small ribbon of smooth muscle known as the muscularis mucosae. The muscularis mucosae are at the border between the inner mucosa and outer submucosa and create folds in the stomach and to optimize the surface for digestion and absorption.
The tunica submucosa is sandwiched in between the inner mucosa and outer muscularis externa layer. You will notice by looking at the image that this layer contains yet more blood vessels, lymphatics, and nerves. It contains a grouping of nerves known as the ; these nerves innervate cells lining the GI tract, as well as the smooth muscle of the muscularis mucosae, controlling local secretions, absorption, and muscle movements.
The muscularis externa layer, as the name implies consists primarily of smooth muscle. It is important to note that along the entire GI tract the muscularis externa consists of two distinct muscular layers that run perpendicular to each other: the inner circular and outer longitudinal. The circular muscle layer fibers wrap around the circumference of the organ. The outer longitudinal muscle layer runs lengthwise down the GI tract. Contraction of muscle along these two layers helps break down food mechanically, mix it with digestive secretions and propel it through the tract. These peristaltic contractions that squeeze substances through the GI tract are orchestrated by a grouping of enteric nerves sandwiched in between the circular and longitudinal layer known as the .
The GI tract’s outermost layer (visceral peritoneum) is known as the serosa layer. It covers most of the GI tract within the peritoneal cavity, but there is no serosa covering the muscularis externa of the oral cavity, , esophagus, and . These areas are anchored to adjacent structures by a dense irregular network of collagen fibers called the adventitia.
Peristalsis
Food is pushed from the oral cavity through the entire GI tract through a coordinated series of smooth muscle contractions known as . It is thought that the gastrointestinal tract contains more neurons than the entire spinal cord. These nerves that make up the submucosal and myenteric plexus are part of the third branch of the autonomic nervous system (the enteric nervous system) and are essential to orchestrate the churning, mixing, and of food that facilitates its digestion and absorption.
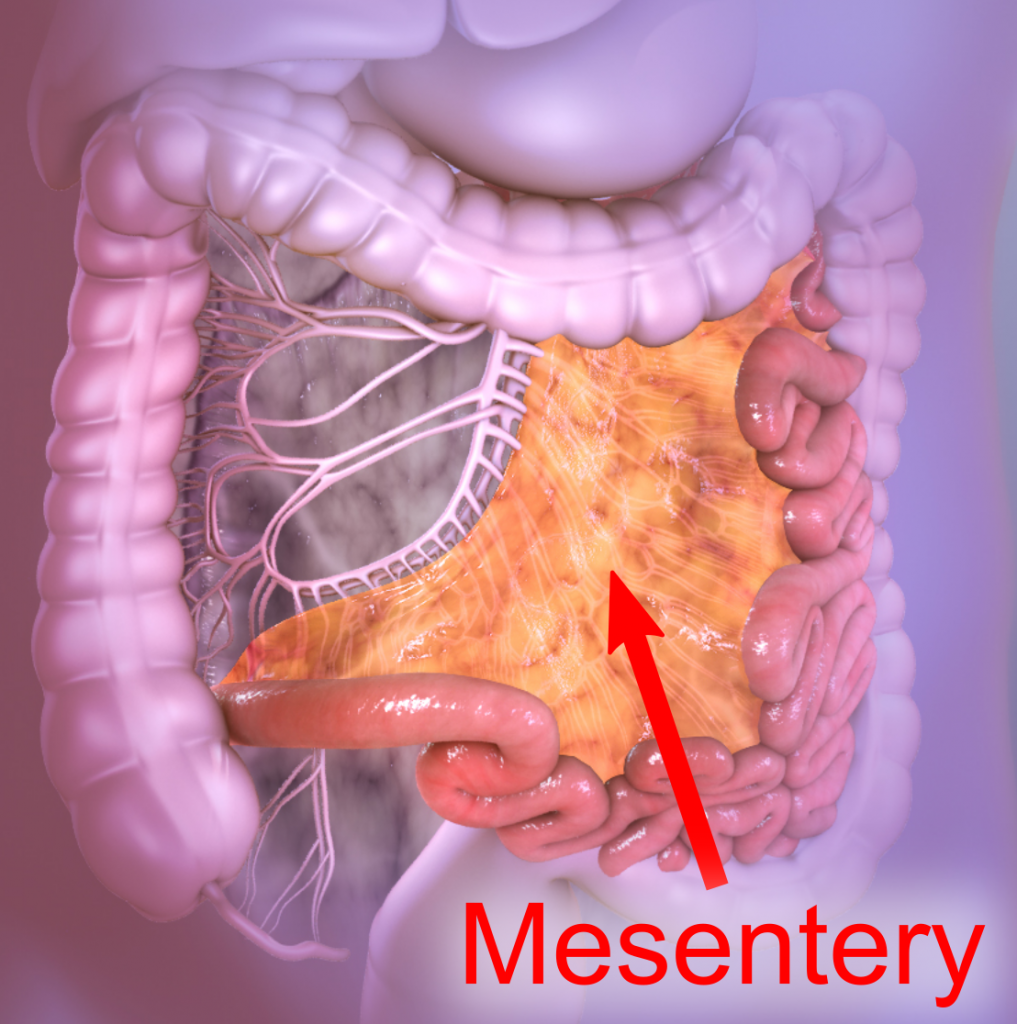
Mesenteries
 |
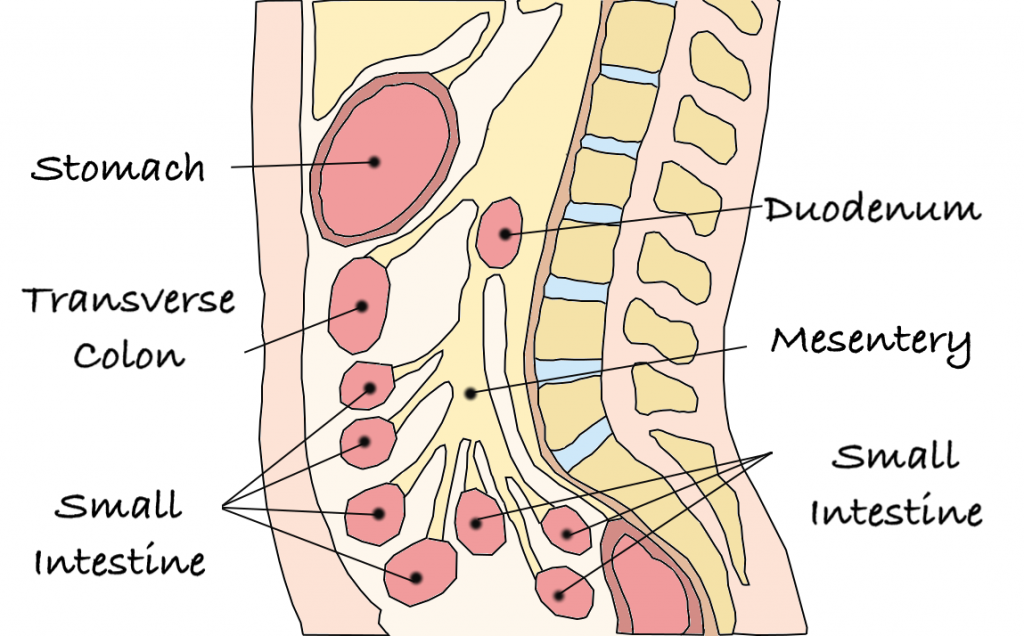 |
Figure 23.6: Mesenteries
The parietal peritoneum that lines the inner surfaces of the peritoneal or abdominopelvic cavity is continuous with the serosa of the GI tract. The peritoneum is constantly producing a lubricating fluid to the peritoneal surfaces. Within the peritoneal cavity, most regions of the GI tract are suspended by peritoneum extensions called mesenteries. These are double sheets of the peritoneum with areolar tissue sandwiched in between. Keep in mind that the overall outcome of the digestive system is to facilitate the absorption of nutrients into the bloodstream and lymphatics. It would logically follow that a passageway for arteries, veins, lymph vessels, and nerves be provided to these areas. The mesenteries provide such a passageway. Furthermore, mesenteries act to secure the position of the GI tract in the peritoneal cavity. They also permit the necessary movement of this muscular tube within the cavity. There are organs of the peritoneal cavity that lie behind the peritoneal membrane. These organs are said to be in the space. These retroperitoneal organs are secured against the back wall of the peritoneal cavity. They include the kidneys, the , a portion of the , the spleen, and the lower . Prominent portions of the mesenteries are the lesser omentum which suspends the stomach and provides a route for blood vessels, lymphatics, and nerves to and from the stomach, and the greater omentum, which has been described as a bib-like structure hanging from the inferior portion of the stomach. The greater omentum contains adipose tissue that cushions the deeper organs in the abdominal area. As a person gains weight this structure can increase its fat reserves, size, and thickness. The majority of the small intestine is suspended by the mesentery proper and most of the large intestine is suspended by a sheet of mesentery known as the mesocolon.
Digestive System Processes
The processes of digestion include six activities: , propulsion, mechanical or physical digestion, , absorption, and .
The first of these processes, ingestion, refers to the entry of food into the alimentary canal through the oral cavity (mouth). In the mouth, the food is chewed and mixed with . The saliva contains enzymes that begin breaking down the carbohydrates in the food. In addition, a small amount of lipid chemical breakdown takes place due to released by epithelium on the surface of the . Chewing increases the surface area of the food and allows an appropriately sized to be produced.
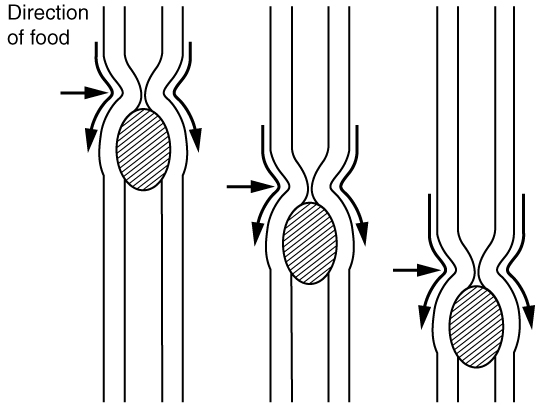
Food leaves the mouth when the tongue and pharyngeal muscles propel it into the esophagus. This act of swallowing is an example of propulsion, which refers to the movement of food through the digestive tract. It includes both the voluntary processes like swallowing and involuntary processes like peristalsis. Peristalsis consists of sequential, alternating waves of contraction and relaxation of alimentary wall smooth muscles, which act to propel food along. These waves also play a role in mixing food with digestive juices. Peristalsis is so powerful that foods and liquids you swallow enter your stomach even if you are standing on your head.
 |
 |
| Peristalsis moves food through the digestive tract with alternating waves of muscle contraction and relaxation. (OpenStax fig 23.5 link) | The esophagus transfers food from the mouth to the stomach through peristaltic movements. OpenStax Bio AP |
Figure 23.7 Peristalsis
This image shows the peristaltic movement of food. In the left image, the food bolus is towards the top of the esophagus and arrows pointing downward show the direction of movement of the peristaltic wave. In the center image, the food bolus and the wave movement are closer to the center of the esophagus and in the right image, the bolus and the wave are close to the bottom end of the esophagus.
Digestion includes both mechanical and chemical processes. is a purely physical process that does not change the chemical nature of the food. Instead, it makes the food smaller to increase both surface area and mobility. It includes , or chewing, as well as tongue movements that help break food into smaller bits and mix food with saliva. Although there may be a tendency to think that mechanical digestion is limited to the first steps of the digestive process, it occurs after the food leaves the mouth, as well. The mechanical churning of food in the stomach serves to further break it apart and expose more of its surface area to digestive juices, creating an acidic “soup” called . , which occurs mainly in the small intestine, consists of localized contractions of circular muscle of the muscularis layer of the alimentary canal. These contractions isolate small sections of the intestine, moving their contents back and forth while continuously subdividing, breaking up, and mixing the contents. By moving food back and forth in the intestinal lumen, segmentation mixes food with digestive juices and facilitates absorption.
In chemical digestion, starting in the mouth, digestive secretions break down complex food molecules into their chemical building blocks (for example, proteins into separate amino acids). These secretions vary in composition but typically contain water, various enzymes, acids, and salts. The process is completed in the small intestine.
Food that has been broken down is of no value to the body unless it enters the bloodstream and its nutrients are put to work. This occurs through the process of absorption, which takes place primarily within the small intestine. There, most nutrients are absorbed from the lumen of the alimentary canal into the bloodstream through the epithelial cells that make up the mucosa. Lipids are absorbed into s and are transported via the lymphatic vessels to the bloodstream (the subclavian veins near the heart). The details of these processes will be discussed later.
Defecation is the final step in digestion, in which undigested materials are removed from the body as .
Regulatory Mechanisms
Neural and endocrine regulatory mechanisms work to maintain the optimal conditions in the lumen needed for digestion and absorption. These regulatory mechanisms, which stimulate digestive activity through mechanical and chemical activity are controlled both extrinsically and intrinsically.
Neural Controls
The walls of the alimentary canal contain a variety of sensors that help regulate digestive functions. These include mechanoreceptors, chemoreceptors, and osmoreceptors, which can detect mechanical, chemical, and osmotic stimuli, respectively. For example, these receptors can sense when the presence of food has caused the stomach to expand, whether food particles have been sufficiently broken down, how much liquid is present, and the type of nutrients in the food (lipids, carbohydrates, and/or proteins). Stimulation of these receptors provokes an appropriate reflex that furthers the process of digestion. This may entail sending a message that activates the glands that secrete digestive juices into the lumen, or it may mean the stimulation of muscles within the alimentary canal, thereby activating peristalsis and segmentation that move food along the intestinal tract.
The walls of the entire alimentary canal are embedded with nerve plexuses that interact with the central nervous system and other nerve plexuses — either within the same digestive organ or different ones. These interactions prompt several types of reflexes. Extrinsic nerve plexuses orchestrate long reflexes, which involve the central and autonomic nervous systems and work in response to stimuli from outside the digestive system. Short reflexes, on the other hand, are orchestrated by intrinsic nerve plexuses within the alimentary canal wall. These two plexuses and their connections were introduced earlier as the enteric nervous system. Short reflexes regulate activities in one area of the digestive tract and may coordinate local peristaltic movements and stimulate digestive secretions. For example, the sight, smell, and taste of food initiate long reflexes that begin with a sensory neuron delivering a signal to the medulla oblongata. The response to the signal is to stimulate cells in the stomach to begin secreting digestive juices in preparation for incoming food. In contrast, food that distends the stomach initiates short reflexes that cause cells in the stomach wall to increase their secretion of digestive juices.
Hormonal Controls
A variety of hormones are involved in the digestive process. The main digestive hormone of the stomach is , which is secreted in response to the presence of food. Gastrin stimulates the secretion of gastric acid by the s of the stomach mucosa. Other GI hormones are produced and act upon the gut and its accessory organs. Hormones produced by the duodenum include secretin, which stimulates a watery secretion of bicarbonate by the pancreas; cholecystokinin (CCK), which stimulates the secretion of pancreatic enzymes and from the and release of bile from the ; and gastric inhibitory peptide, which inhibits gastric secretion and slows and . These GI hormones are secreted by specialized epithelial cells, called endocrinocytes, located in the mucosal epithelium of the stomach and small intestine. These hormones then enter the bloodstream, through which they can reach their target organs.
The structure and function of organs and accessory organs making up the digestive system will be presented in chronological order as food would move through the GI tract.
23.2 Oral Cavity
![]() 23.2 Learning Objectives
23.2 Learning Objectives
- Describe the structures of the mouth, including its accessory digestive organs
- Group adult teeth according to name, location, and general function
- Describe what saliva is, how it is produced, and its general functions in digestion
- Trace the pathway food follows from ingestion into the mouth and into the pharynx
Ingestion of food starts in the oral cavity. The oral cavity contains the teeth, s, the tongue, and chemical taste receptors. Both mechanical and chemical digestion of macromolecules begins in the oral cavity. The process of mastication (chewing) starts to mechanically break up the food being eaten. Keep in mind that to be absorbed food must be broken down into its most simple components. The process of chewing starts to break larger chunks of food into smaller and smaller bits. This process is important because as the food is broken down it increases the surface area for chemical digestion to take place. During the process of mastication, the various salivary glands produce and release saliva into the oral cavity. Chewing and churning the food in your mouth with the use of the teeth and tongue helps to mix the saliva into the food. This process moistens food, begins some enzymatic digestion, and prepares it for swallowing.
Oral cavity anatomy and landmarks
The oral cavity (mouth) is lined with oral mucosa which is composed of stratified squamous epithelium. The majority of surface area within the oral cavity is the nonkeratinized squamous epithelium, however, the keratinized epithelium is located in areas of abrasion such as the surface of the tongue and oropharynx. The anterior portion of the oral cavity is guarded by the labia (lips). The lateral portion of each side of the mouth is composed of soft tissue known as the cheeks, which contain fat and the buccinator muscles. The buccinator muscles act to compress the cheek aiding in the churning of food while chewing in the oral cavity. The teeth are anchored into the upper and lower jaw via the alveolar processes. The alveolar processes are covered by a mucosae layer called the (gums).
 |
 |
Figure 23.8: Mouth, Oral cavity anterior and lateral view
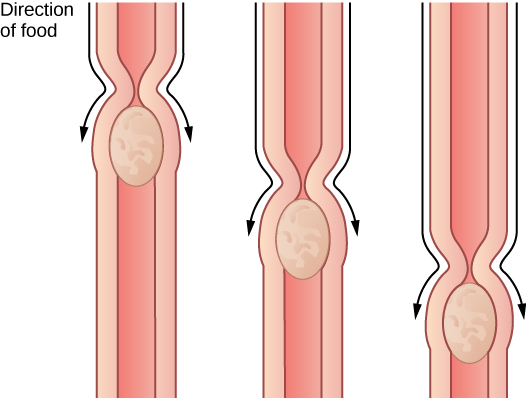
Salivary Glands
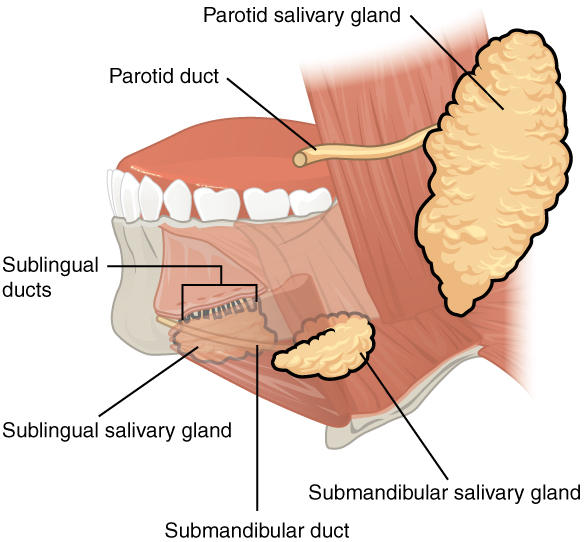
Figure 23.9 Salivary glands from OpenStax
Saliva is produced by 3 pairs of salivary glands that empty into the oral cavity via ducts. The parotid salivary glands are situated anterior to the ear lobes and deep into the skin. They release saliva that contains . Recall any word ending with “-ase” is an enzyme. The enzymes in salivary amylase act to enzymatically break down complex carbohydrates into simple sugars. As the complex carbohydrates are broken down into simple sugars, the chemoreceptors in your tastebuds register the food being chewed becoming sweeter. Recall chewing on pizza dough for a long period. After a while, it tastes sweeter. The submandibular salivary glands are situated medial to the mandible and contain smaller amounts of salivary amylase. Finally, the sublingual salivary glands lie deep in the tongue and contribute to the volume of saliva.
Salivary secretions are influenced by the autonomic nervous system. Putting food in your mouth can trigger the salivary reflex. This triggers the salivary glands to produce and release copious amounts of saliva. Furthermore, just thinking about food, or smelling food can trigger this salivary reflex.
The Teeth
Teeth are involved in the process of mastication (chewing). They are essential for shearing and grinding food. In addition, mastication helps to mix salivary secretions with the food being chewed.
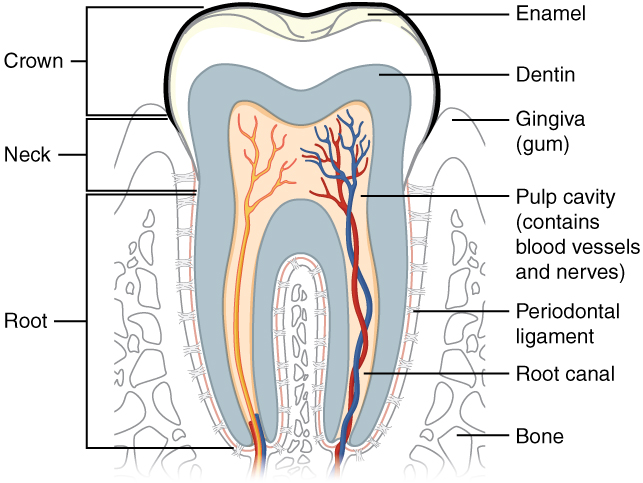
Figure 23.10 The Structure of the Tooth from OpenStax
The superior portion of each tooth projecting from the gingiva is made of an extremely hard outer layer known as . Enamel is thought to be the hardest biologically produced substance. Within the enamel of the tooth is a mineralized matrix known as . This substance is similar to the bone matrix; however, it lacks cells associated with bone. The blood and nerve supply to the tooth is provided by the canal which allows the penetration of blood vessels and nerves into a central area of the tooth (deep to the dentin) known as the . The root of each tooth fits into a bony socket called an alveolus. Here collagen fibers making up the periodontal ligament produce a rigid immovable attachment between tooth and jaw known as a gomphosis joint. There are three basic portions of a tooth. The crown is the exposed portion of the tooth that has an outer enamel layer. The root sits below the gingival line and acts to anchor the tooth to the jaw and the neck which sits between the crown and the root.
Types of Teeth
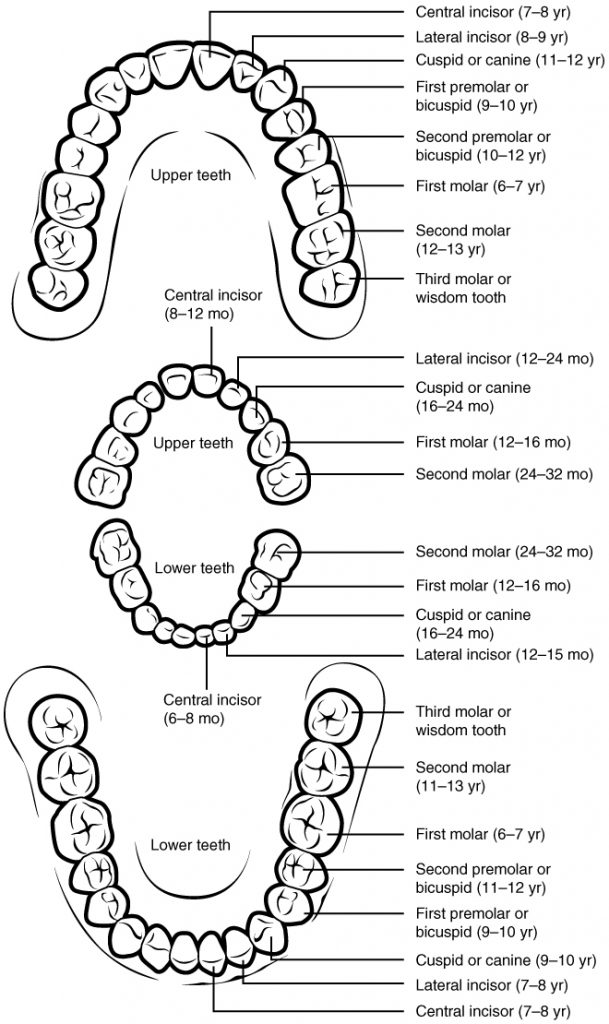
Figure 23.10 Permanent and Deciduous Teeth from OpenStax
A typical adult mouth contains 32 teeth. These can be divided into 4 general categories:
- s serve as grinders. They have rather flat surfaces and are found in the posterior region of the upper and lower jaws.
- Bicuspids are anterior to the molars they also are involved with crushing and grinding.
- The s (canines) have more of a cone shape to them. They are designed for tearing.
- The s are used for shearing food to bring into your mouth, for example biting off a corner of a sandwich.
Deciduous Teeth
As we all know most babies are born without teeth, and throughout child development, the teeth grow in. In addition, children will end up losing their 20 deciduous (baby) teeth as the secondary teeth erupt from the jaw. As the secondary teeth grow in, the enlarged jaw (due to both intramembranous and endochondral ossification) leaves room for three additional molars to develop on the upper and lower jaw. This brings the total number of secondary teeth (adult teeth) to 32.
The Tongue
The tongue is a muscular organ that serves to manipulate food being chewed. It can be divided into a posterior portion (root) and an anterior (body) that occupies the anterior portion of the oral cavity. The tongue contains various mound-like structures on the surface known as lingual papillae. Many of these papillae contain chemoreceptors involved with the sensation of chemicals (taste). The inferior portion of the tongue is anchored by a medial structure known as the which acts to limit the movement of the tongue. There are openings of ducts from salivary glands on each side of the base of the lingual frenulum. The epithelium of the tongue contains glands that produce a small amount of lingual lipase. This enzyme acts to break down fatty acids and continues this digestion when the food is moved into the stomach.
23.3 Pharynx
![]() 23.3 Learning Outcomes
23.3 Learning Outcomes
By the end of this section, you will be able to:
- Name, identify, and describe the gross anatomical structures of the pharynx and its regions
- Describe the process of swallowing (deglutition), including the roles of the tongue, , and epiglottis
 |
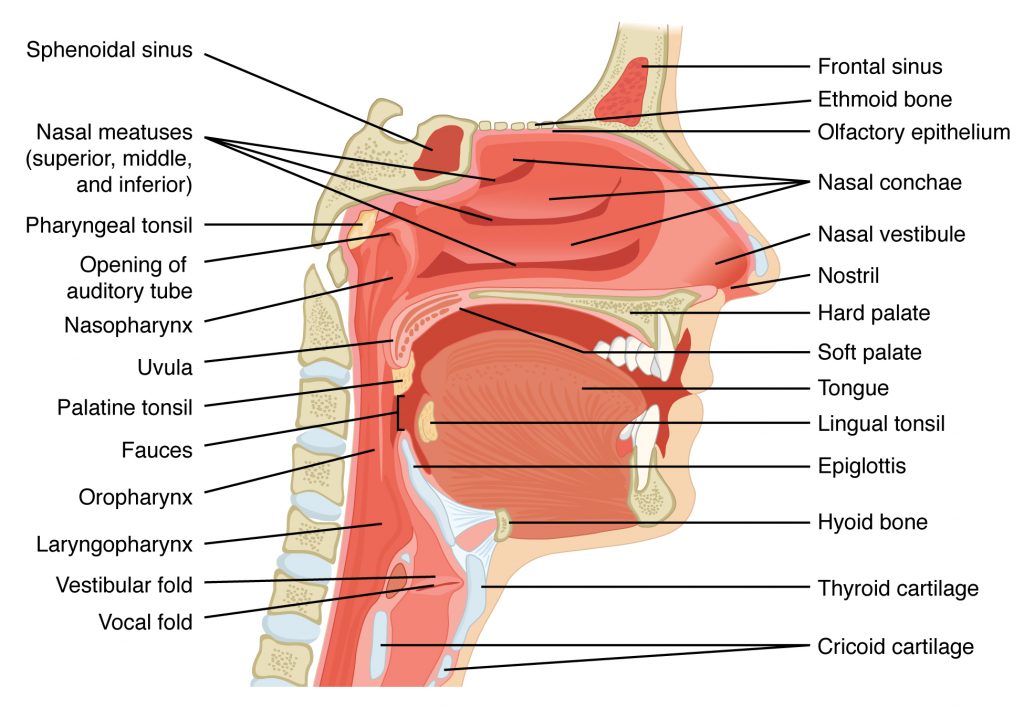 |
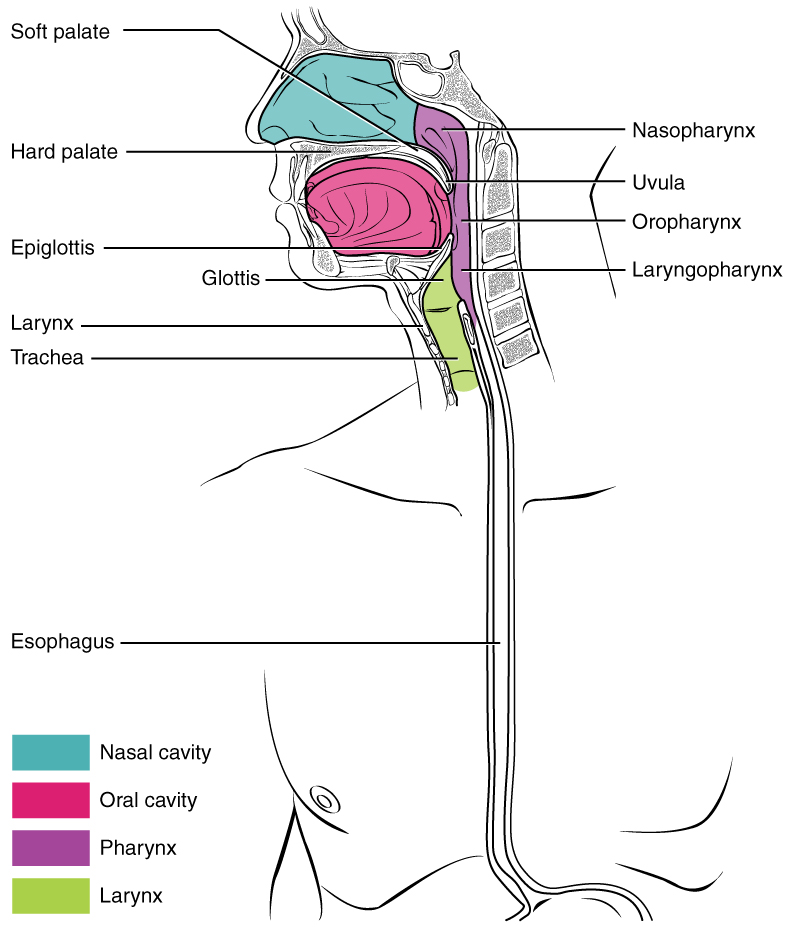
Figure 23.11: Pharynx
Once the food is properly chewed it is ready to enter the pharynx to be swallowed. The pharynx (throat) is a space that is a passageway for food, liquid, and air. The pharynx can be divided into the nasopharynx, oropharynx, and . However, when food is swallowed it passes first from the oral cavity through the oropharynx and laryngopharynx, and then to the esophagus. Stratified squamous epithelium lines the region of the pharynx where food passes through.
(swallowing) is the process of transferring food from the oral cavity to the esophagus. It begins as a voluntary process, however the complex series of events that take place after the initial voluntary process is an autonomic reflex known as the swallowing reflex. When food is voluntarily pushed against the posterior palate of the oral cavity it triggers a complex series of contractions of musculature in the pharynx diverting food to the esophagus. It is important to note that the series of muscular contractions elevates the pharyngeal structures in turn causing the epiglottis to cover the opening to the trachea. This important motion diverts food and liquid to the esophagus preventing them from entering the trachea.
23.4 Esophagus
![]() 23.4 Learning Outcomes
23.4 Learning Outcomes
By the end of this section, you will be able to:
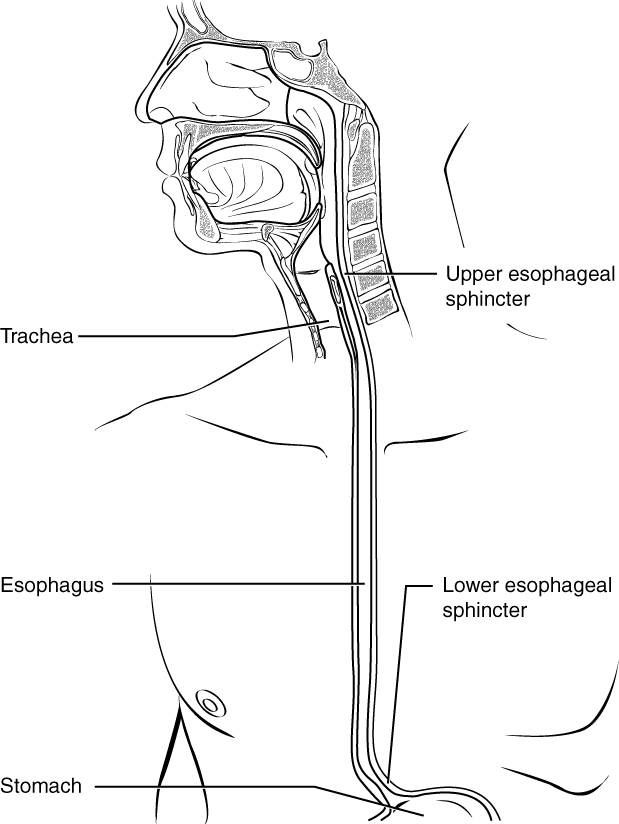
- Locate where the esophageal sphincters are and explain their importance in the control of digestion
- Describe the process of peristalsis and how it propels food through the esophagus
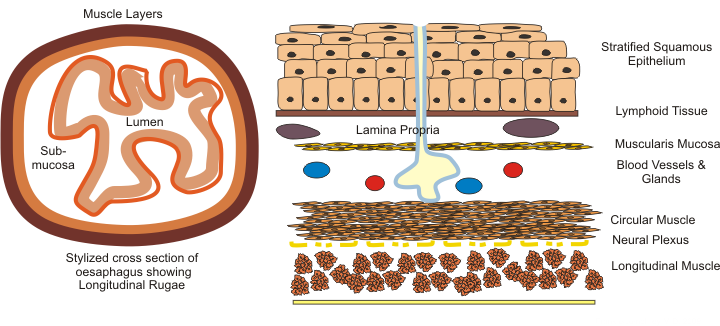
- Describe the histology of the walls of the esophagus
 |
|
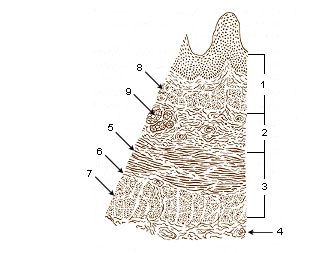 |
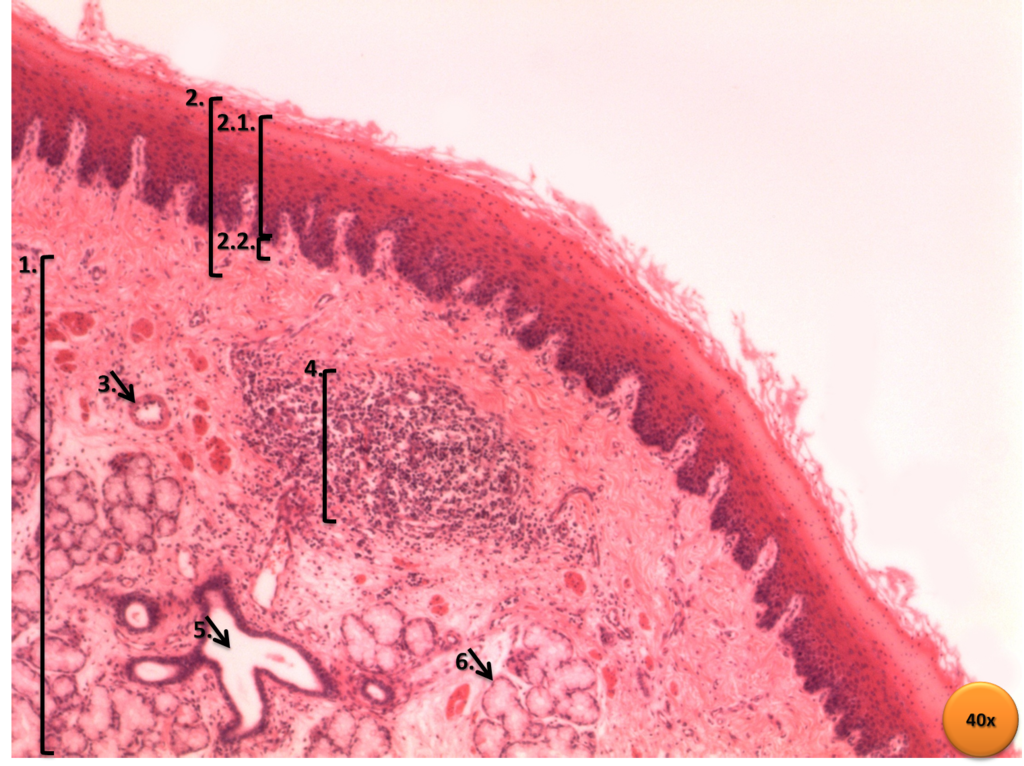
Layers of Esophageal Wall
|
 |
|
| Esophagus Histology: 1.Submucosal layer 2.Mucosal layer 2.1. Non-keratinized stratified squamous epithelial tissue 2.2. Lamina propria 3.Blood vessel 4.Lymphatic node 5.Excretory duct 6.Mucous gland | |
 |
|
Figure 23.12: Esophagus
The esophagus is a muscular tube that extends from the pharynx to the stomach. It is approximately (depending on a person’s height) 26 cm in length. It runs posterior to the trachea and penetrates the diaphragm at an opening known as the esophageal hiatus. The food that is swallowed from the oral cavity is known as a bolus. The bolus of food is pushed down the esophagus by way of peristaltic contractions from the muscular layer of the esophagus. The mucosa layer of the esophagus is lined with stratified squamous epithelium. The submucosa of the esophagus contains various mucous secreting glands known as esophageal glands, which produce mucous helping to reduce friction between the esophageal lining and substances being swallowed.
Although not prominent, the (c sphincter) is a physical barrier that helps to block contents from the stomach going retrograde (backward) and back up into the esophagus.
23.5 Stomach
![]() 23.5 Learning Outcomes
23.5 Learning Outcomes
By the end of this section, you will be able to:
- Label, on a diagram, the four main regions of the stomach, their curvatures, and the sphincter
- Identify the main types of secreting cells in gastric glands, their products, and roles in aiding digestion and the function of the stomach
- State examples of how the stomach protects itself from the chemical digestive processes occurring within itself
- Describe the mechanical and chemical digestion of food entering the stomach
Once a bolus is pushed along the esophagus it is deposited into the stomach. The stomach is a J-shaped organ that serves in the storage of ingested food. The stomach is involved with the further mechanical and chemical breakdown of food, and the production of a glycoprotein known as an that is essential for the absorption of a component critical in the production of red blood cells known as vitamin B12. Keep in mind, that it is in the stomach that chemical and mechanical digestion of foodstuffs is accelerated. The extra muscle layer of the stomach (discussed later) helps to churn and further mix ingested material with stomach secretions.
Anatomy of the stomach
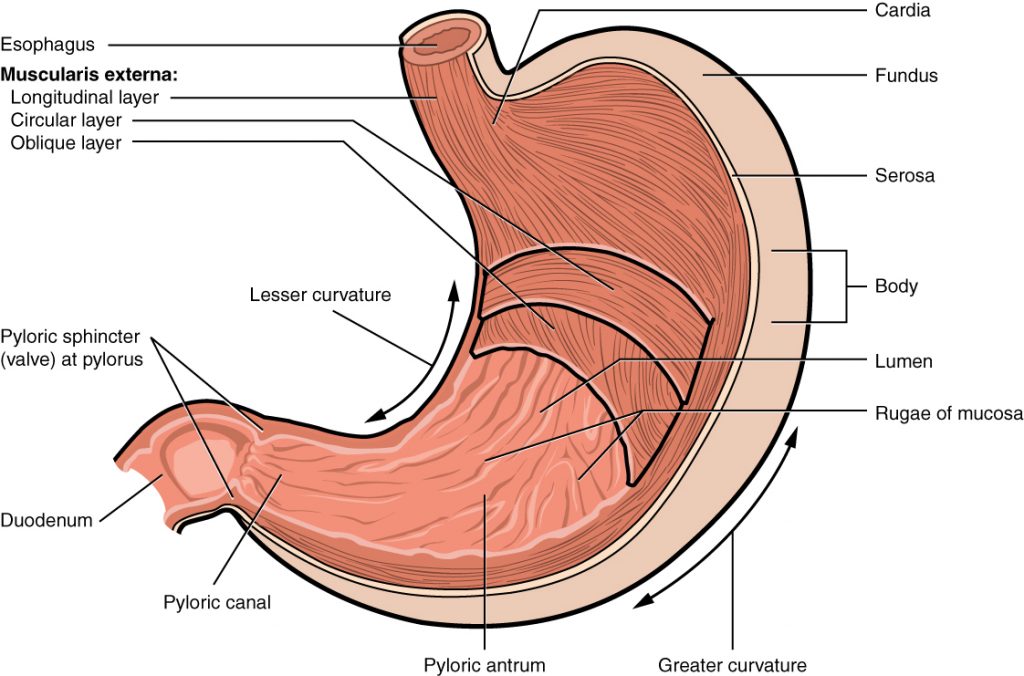
Figure 23.13: Stomach: Gross anatomy of the stomach — coronal cut [from OpenStax]
The stomach is divided into 4 major regions. The cardia, , body, and . Each region is anatomically and physiologically unique.
The cardia is the superior portion of the stomach where the esophagus joins. It contains mucous glands which produce a protective coating lining this area.
The fundus of the stomach is the most superior portion of the stomach. It usually contains gasses.
The body of the stomach represents the largest portion and serves as a holding tank for ingested food and liquid. It also contains most of the gastric secretions described later in this chapter.
Finally, the pyloric region of the stomach makes up the inferior portion where the stomach meets with the first part of the small intestine, the duodenum. At this junction there is a true sphincter muscle serving as a gatekeeper between the junction of the stomach and the duodenum and this is known as the .
![]() Clinical Application
Clinical Application
Pyloric Stenosis
Pyloric Stenosis is a condition that typically takes place in infancy. It is the most frequent condition requiring surgery in infants. Hypertrophic Pyloric Stenosis typically starts a few weeks after birth, it results in the thickening of the pyloric sphincter. As a result, the contents of the stomach are not readily moved from the stomach to the duodenum. The result of this can be forceful vomiting of the infant. Pyloric stenosis can lead to dehydration and malnutrition as the infant has trouble moving food from the stomach to the duodenum.
Notice the various folds that are unique to only the stomach. These folds are known as e. As the stomach fills with food or liquid, the stomach can expand, increasing in size, as the rugae unfold and disappear.
Histology and layers of the stomach wall
As we will learn, the pH within the stomach is low providing for very harsh acidic conditions. With that in mind, the mucosa layer of the stomach needs to produce copious amounts of alkaline mucus to line and protect the layers of the stomach from harsh stomach contents. This mucous epithelium consists of simple columnar epithelium.
Stomach Layers
As stated earlier the stomach, being part of the GI tract, will contain the four distinct layers that are found throughout the GI tract. It is interesting to note that the muscularis externa layer of the stomach contains an EXTRA intermittent inner layer of muscle known as the oblique muscle layer. This muscle is essential for the contractions of the stomach that aid in the churning and mixing of chyme (food that has entered the stomach and mixed with stomach secretions).
Gastric Glands/Pits
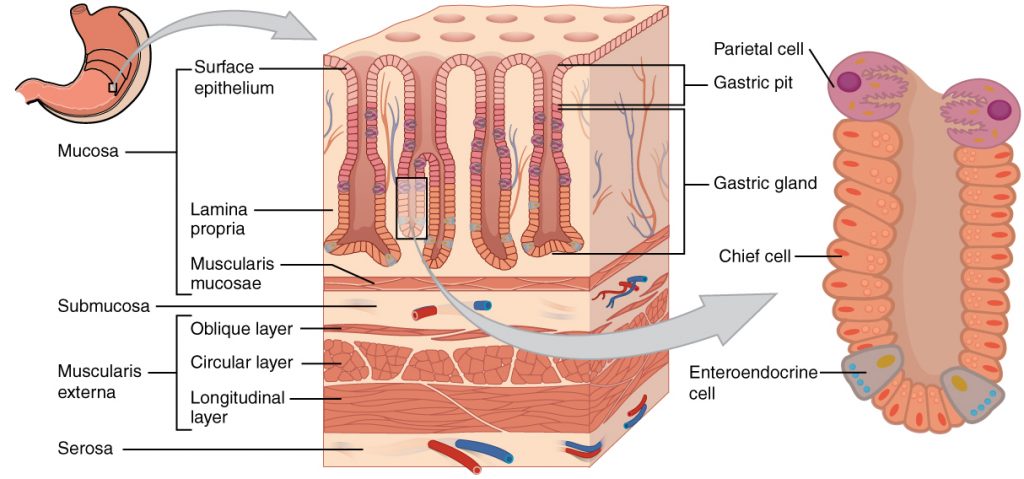
Figure 23.14: Gastric Gland/Pit [from OpenStax]
The prominent mucosa layer of the stomach contains invaginations of the epithelium called s that contain an abundance of secreting cells known collectively as s. Three separate types of cells are found in the gastric glands. Parietal cells, s, and s.
Parietal cells
Parietal cells secrete intrinsic factor and hydrogen and chloride ions. Intrinsic factor (mentioned earlier) is a glycoprotein that aids in the absorption of vitamin B12 from the diet.
Parietal cells produce hydrochloric acid through a clever process. They combine the carbon dioxide they produce with water to form carbonic acid. This carbonic acid dissociates into bicarbonate and hydrogen ions. The hydrogen ions are actively (using ATP) pumped out of the cell into the lumen (opening) of the stomach. In addition, chloride ions are pumped into the cell from the apical surface and diffuse across the cell into the luminal contents of the stomach. In the stomach, the hydrogen ions and chloride ions form , a strong acid.
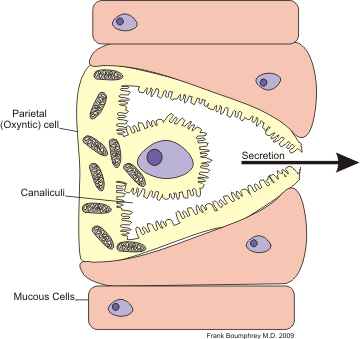 |
 |
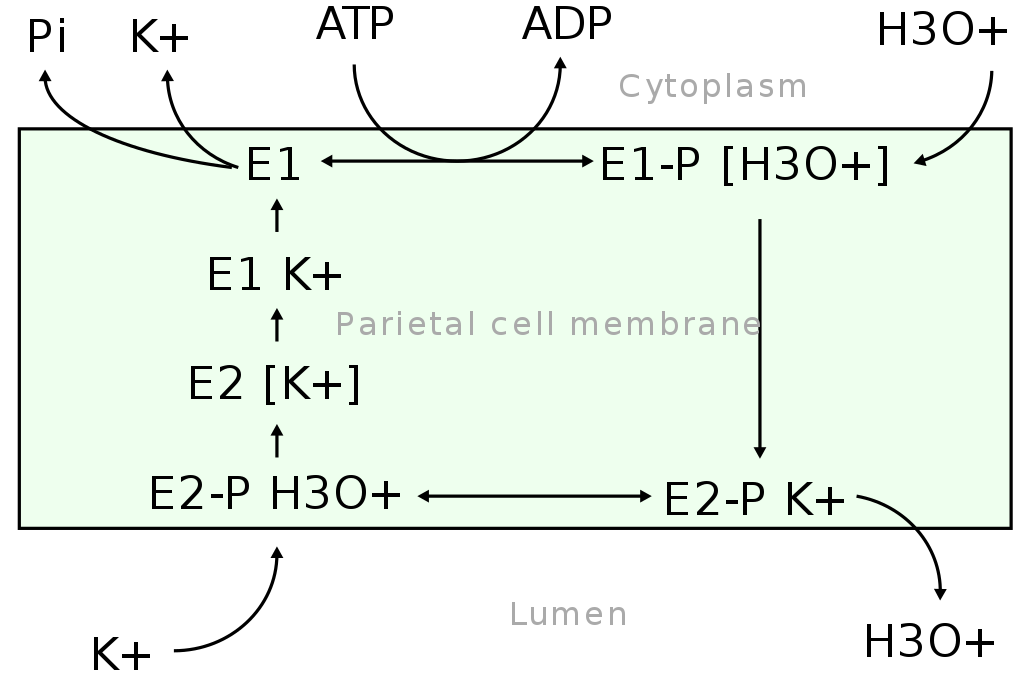 |
| Parietal cell secretion | Parietal cell chemistry | Mechanism of the gastric H+/K+ ATPase within parietal cells showing how E1-E2 conformational changes lead to ion release and stomach acid (HCl) formation |
Figure 23.15: Parietal cell secreting HCL
Hydrochloric acid lowers the pH of the stomach (increases the acidity). The pH of the stomach can drop below 2. This extremely acidic environment of the stomach serves several purposes. 1. It helps to neutralize and kill various microorganisms that may be ingested. 2. It helps to accelerate the chemical breakdown of macronutrients. It serves to denature proteins and digest plant cell walls. 3. It acts to facilitate the conversion of to pepsin (an enzyme that acts to break down larger proteins into individual amino acids.) This conversion only takes place in an acidic environment.
Chief Cells
Chief cells which are found deeper in the gastric glands secrete a proenzyme pepsinogen, which is an inactive form of pepsin, a powerful enzyme that breaks peptide bonds between amino acids (breaks down proteins). Once secreted into the stomach lumen, the highly acidic environment of the stomach facilitates the conversion of pepsinogen to pepsin. Pepsin is most active at a pH below 2.
G Cells
G Cells are abundant along with the gastric pits in the pyloric region of the stomach. These are considered s and produce a cocktail of hormones. The most prominent of these hormones is known as gastrin. An abundance of chyme within the stomach triggers the G cells to produce gastrin. Gastrin, in turn, stimulates the activity level of the stomach to accelerate mechanical and chemical digestion. It does so by activating muscular contractions of the stomach as well as increasing the activity and secretion of parietal and chief cells.
Regulation of stomach activity
Regulation of gastric activity is a complex process that involves input from the central nervous system, hormones produced by the digestive tract, and short reflexes from the enteric nervous system.
Summary of absorption and digestion in the stomach
As stated earlier digestion of foodstuffs accelerates drastically in the stomach, however, very little nutrient absorption takes place here. As one swallows a meal, the pH of the chyme entering the stomach will progressively drop as parietal cells are stimulated to increase their hydrochloric acid production. The amylases and lipases from the mouth will continue to chemically digest carbohydrates and fats respectively until the pH of the stomach falls below 4.5. Once the pH reaches 2 or lower, pepsinogen becomes more active and the enzymatic breakdown of proteins continues. However, it is important to note that although digestion of food is accelerated in the stomach, it is far from complete and, overall, no nutrient absorption takes place in this organ. As the histology of the mucosa lining of the stomach demonstrates, the stomach is not designed to absorb nutrients. The columnar cells are covered in a thick layer of alkaline mucus, in addition, they lack the various transport mechanisms to facilitate absorption. The stomach, however, can absorb certain substances. Alcohol and aspirin are two notable exceptions. Both are lipid-soluble and can cross the mucosa lining of the stomach and enter the bloodstream.
Overall Gastric Activity Regulation
The Cephalic Phase
Imagine walking into your favorite restaurant and smelling the delicious food. You have already entered the . The cephalic phase begins when an individual starts to think about, smell, or taste food. This phase triggers your stomach to increase its gastric juices secretions. This parasympathetic tone is delivered via the Vagus nerve (CN X) which synapses at the submucosal plexus of the stomach lining. The activation of the submucosal plexus, in turn, stimulates the mucous, chief, parietal, and G cells. In other words, the stomach is prepping to accept food and start the process of digestion.
The Gastric Phase
This phase starts when food is swallowed and enters the stomach. Stretch and chemoreceptors in the stomach further trigger the activity of the submucosal and the myenteric plexus. This accelerates the activity of stomach churning and secretions. There is also a local response when the wall of the stomach is distended. In response to this, histamine is released which further triggers the activity of the parietal cells. The can last for hours as the consumed food is slowly broken down and released into the small intestine.
The Intestinal Phase
This phase can also last hours depending on the amount and type of food ingested. It starts when chyme (a mixture of ingested food, liquid, and gastric juices) begins to enter the first part of the small intestine (the duodenum). It is important to note that the amount of chyme entering the small intestine can be carefully controlled. Too much chyme entering at once will drastically reduce the pH in the duodenum damaging the delicate mucosa layer. Furthermore, digestion of chyme is a time-consuming process, the duodenum can only accept and digest so fast. Factors such as fat content in the chyme dictate the regulatory factors that cause more or less peristaltic contractions pushing chyme into the small intestine.
23.6 Liver
![]() 23.6 Learning Outcomes
23.6 Learning Outcomes
By the end of this section, you will be able to:
- Describe the contributions of the liver that aid in digestion
- Identify features of liver histology that aid in its digestive functions
- State where bile is made, and discuss the composition and function of bile in digestion
- Describe blood flow through the hepatic portal system and trace how nutrients are carried through blood flow to and from the liver
- Summarize other important functions of the liver in addition to its digestive functions
Introduction
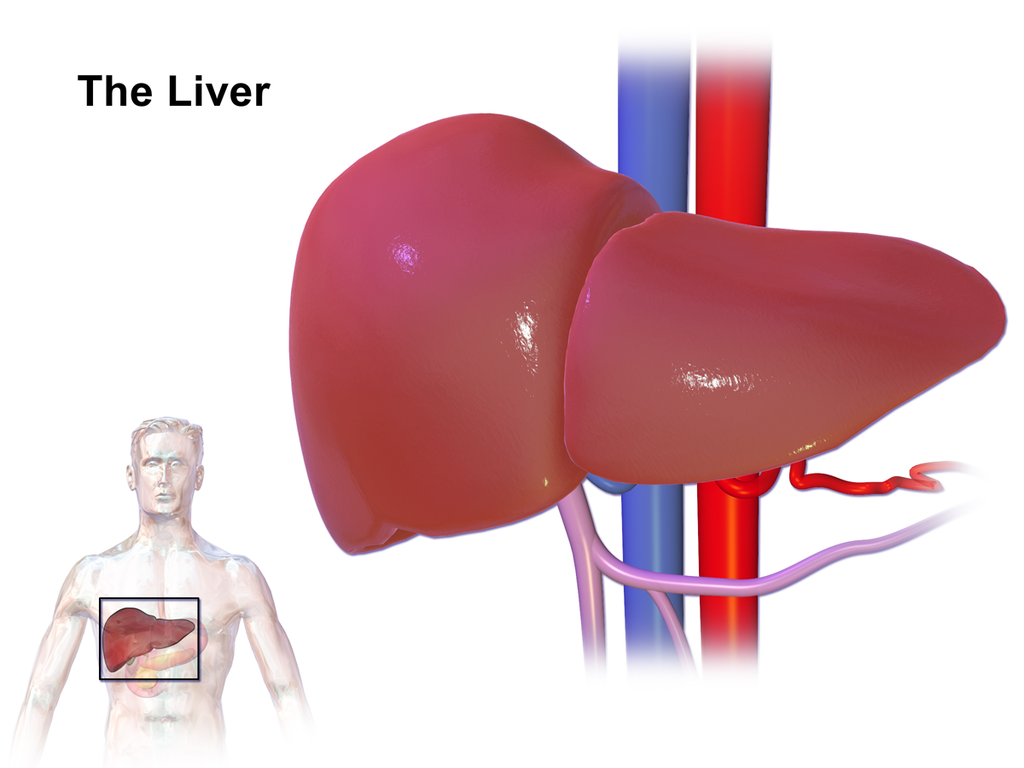
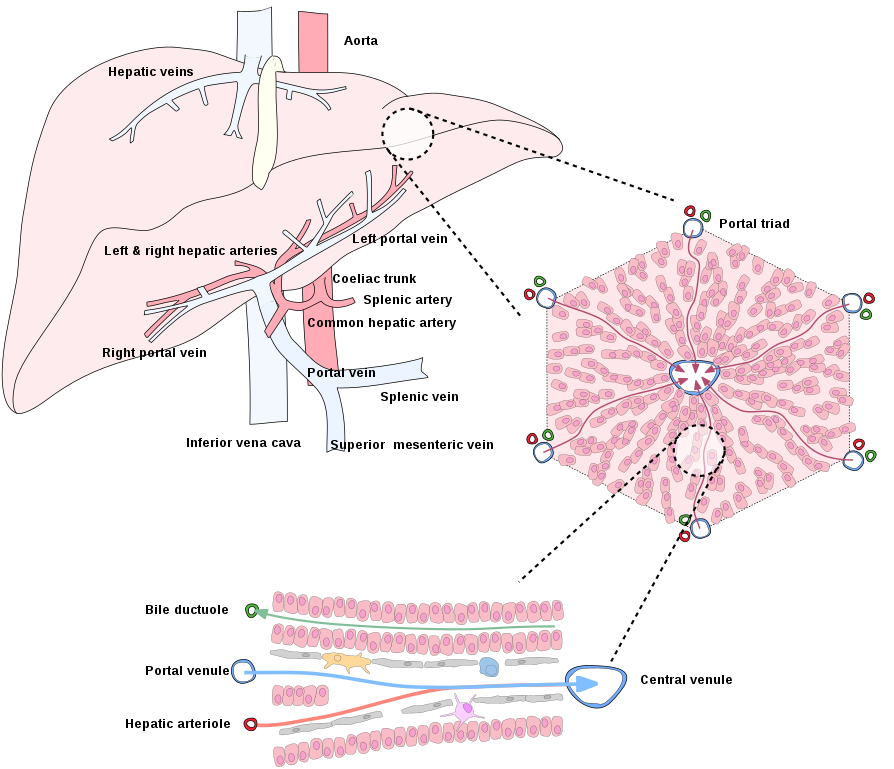
The liver is the largest visceral organ and has over 200 known functions. Its role in digestion and absorption will be discussed in this chapter. The liver is located in the upper right abdominopelvic quadrant directly inferior to the diaphragm. There is a double fold of the peritoneum that suspends the liver known as the falciform ligament. The falciform ligament separates the liver into the right and left lobes. The liver receives blood from two sources, the which supplies oxygen-rich blood, and the which supplies venous blood collected from the majority of the GI tract. When an individual is absorbing a meal, nutrient-rich blood is carried to the liver via the hepatic portal vein. Blood from both the hepatic portal vein and the hepatic artery mix and travel through a network of liver lobules and collect into s which join the s leading to the inferior vena cava. Hepatic circulation will be discussed further in the chapters describing blood vessel configuration.
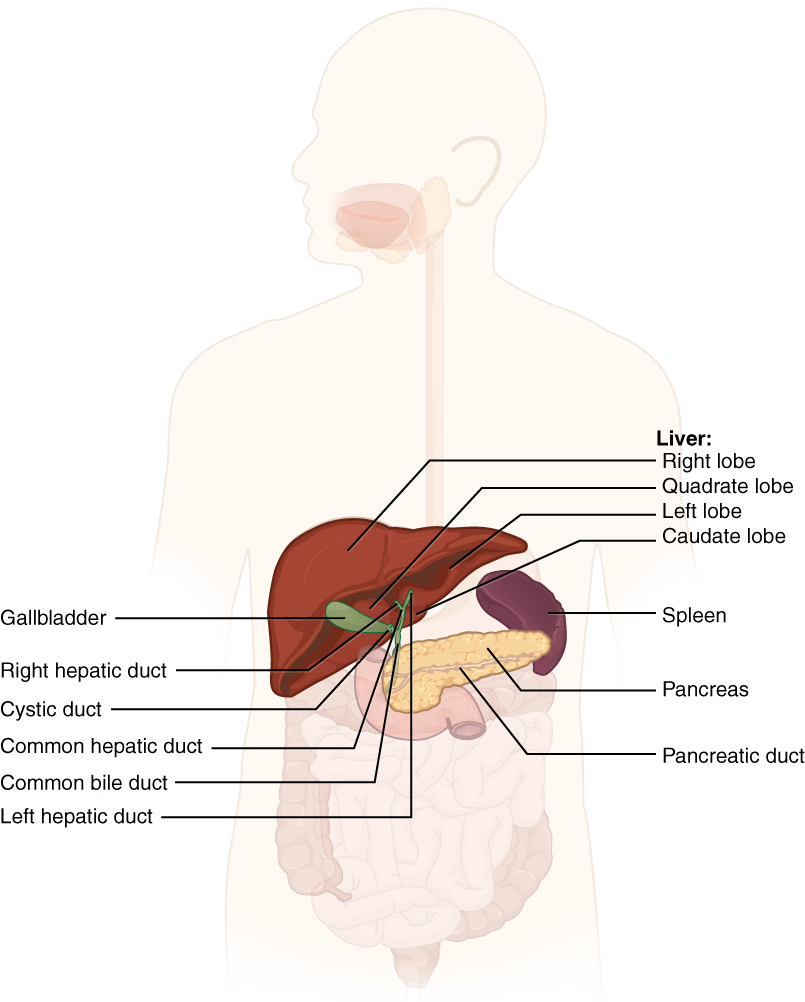 |
 |
|
Accessory Organs The liver, pancreas, and gallbladder are considered accessory digestive organs, but their roles in the digestive system are vital.
|
The Liver |
|
|
Figure 23.16: The Liver
Physiology
It is not coincidental that the veins carrying nutrient-rich blood first run through the lobules of the liver before entering the systemic circulation. Amongst many of the liver functions, it serves to monitor and maintain circulating nutrients and components in the blood. Liver cells () can regulate various nutrients and remove toxins from the blood before it moves through the rest of systemic circulation.
Bile production
Bile consists primarily of water but it also contains , which gives bile a yellow-green color. Bilirubin is a waste product of red blood cell recycling which needs to be eliminated. Other components of bile include cholesterol and bile salts. Bile salts function as a detergent that acts to increase the surface area of fats in the small intestine increasing the surface area for to chemically digest the fats more efficiently.
Carbohydrate metabolism
The liver can extract the absorbed glucose from the bloodstream and store them as a macromolecule known as glycogen. When blood glucose levels drop below the homeostatic minimum, the liver can cleave off individual glucose molecules from glycogen, releasing them into the bloodstream, thus increasing blood glucose levels.
Lipid metabolism
Circulating levels of cholesterol, triglycerides, and fatty acids are also regulated by the liver. These lipid molecules can be stored or packaged in large lipoprotein particles for transport to the rest of the body.
Amino acid metabolism and plasma protein synthesis
Recall from the blood chapter that plasma contains an abundance and variety of plasma proteins. Albumin makes up most of the proteins that are synthesized by the liver, but the liver also produces proteins involved in clotting and hormone transport. Most plasma proteins are manufactured by the liver. The liver extracts amino acids from the nutrient-rich blood supplied by the hepatic portal vein but since amino acids cannot be stored, they need to be used to make protein or be converted to other molecules such as lipids and glucose.
Other liver functions
The liver is involved with many other processes including the removal of bacteria absorbed in the intestines, metabolic waste products, excess circulating hormones, and toxins. The liver is also involved with mineral storage, and drug inactivation.
Bile
As stated earlier, a major contribution of the liver as related to digestion is the production of bile. Hepatocytes of the liver produce approximately one liter (4.2 cups) of bile per day. Although bile is produced by the liver, it is stored and concentrated in the gallbladder. Bile salts are similar to a dishwashing detergent with a polar and nonpolar end. As a detergent bile salts act as an emulsifier of fats. This process is important because pancreatic lipases are most effective and efficient when there is abundant surface area to enzymatically break down fats. When bile is released into the small intestine it can break up a single large fat globule into thousands of tiny droplets. This increase in the surface area promotes the efficiency of lipases. In addition, once the fat is digested, bile salts accelerate the absorption of fat from the small intestine. The majority of bile salts are reabsorbed in the distal part of the small intestine and delivered back to the liver via the hepatic portal vein. This is known as , in which bile salts are recycled and reused.
23.7 Gallbladder
![]() 23.7 Learning Outcomes
23.7 Learning Outcomes
By the end of this section, you will be able to:
- Locate where the gallbladder is in the body and its relation to the liver
- Explain the role of the gallbladder in digestion and bile secretion
As stated earlier in this chapter, bile produced by the liver is transferred to the gallbladder via the . The gallbladder then stores and concentrates bile. When chyme with a high-fat content enters the duodenum, the duodenum releases various hormones including cholecystokinin (CCK) which triggers both the contraction of the gallbladder and the relaxation of the (described in the duodenum section of this chapter) allowing bile to be excreted into the duodenum via the . Occasionally, bile forms gallstones (cholelithiasis) which get stuck in the duct system. This causes a great deal of crampy pain called biliary colic after the ingestion of fatty food triggers contractions of the gallbladder. One of the most common surgical procedures in the country is the removal of the gallbladder in a procedure called a laparoscopic cholecystectomy.
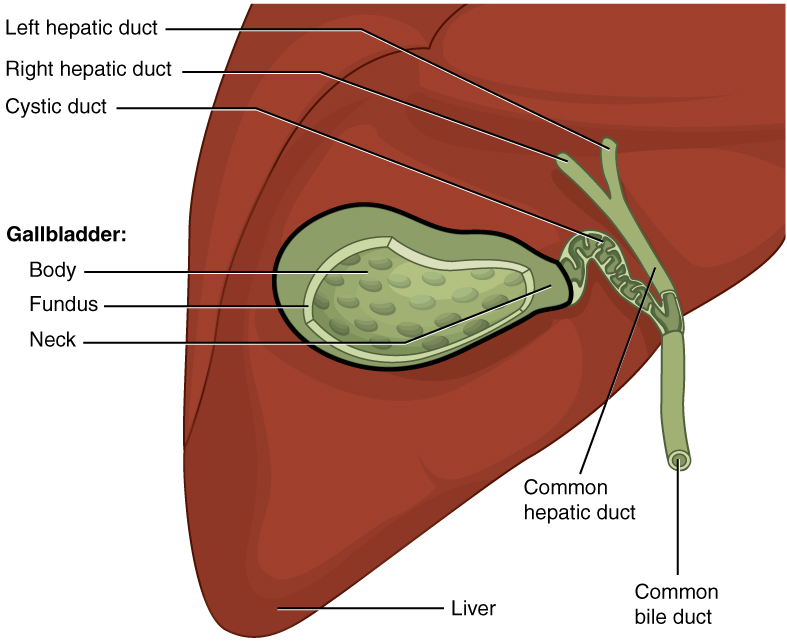
Figure 23.17: Gallbladder OpenStax
![]() Clinical Application
Clinical Application
Removal of the Gallbladder
The removal of the gallbladder (cholecystectomy) may be performed due to gallstones in the gallbladder or the bile duct, gallbladder inflammation, polyps, or constant pancreatitis due to gallstones. As stated earlier, the gallbladder concentrates bile produced by the liver and is used to emulsify fats in the GI tract. Consequently, people who have had gallbladder removal need to be careful with the amount of fat they eat in a meal. Because the removal of the gallbladder will decrease the amount of bile that enters the duodenum, only smaller amounts of fats can be emulsified and broken down. A high-fat meal may result in diarrhea in a person who has had their gallbladder removed.
23.8 Pancreas
![]() 23.8 Learning Outcomes
23.8 Learning Outcomes
By the end of this section, you will be able to:
- Locate the pancreas and describe its anatomy and position relative to other organs
- Describe the exocrine and digestive functions of the pancreas
- Identify the major types of enzymes and buffers present in pancreatic juice
Anatomy of the pancreas
The pancreas is situated in the retroperitoneal space posterior to the stomach and lies transversely as the head is surrounded by the C curvature of the first part of the small intestine (duodenum). The pancreas tapers toward the tail. The pancreas is approximately 15cm (6in.) long. The exocrine secretions are released into small ducts that feed into the pancreatic duct. The pancreatic duct merges with the common bile duct at the hepatopancreatic sphincter in the wall of the duodenum.
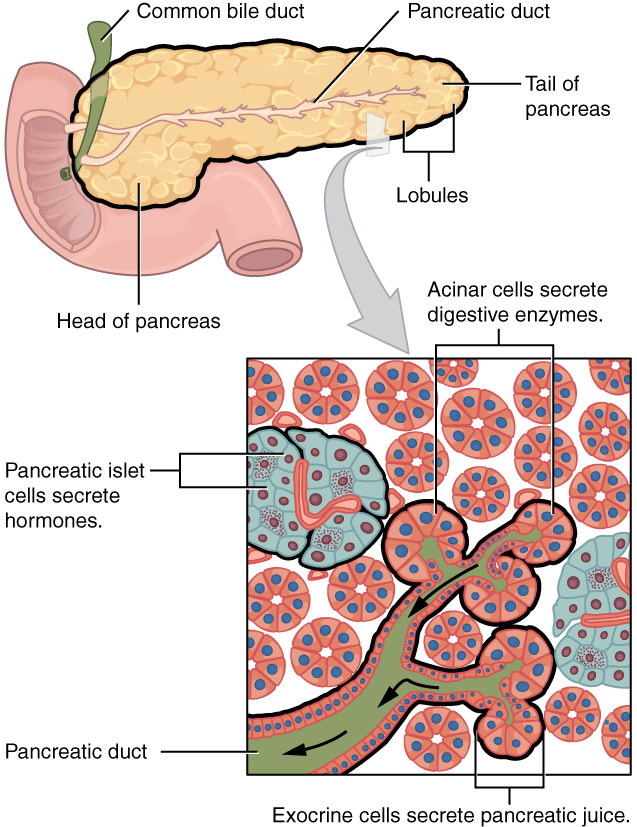 |
| Exocrine and Endocrine Pancreas The pancreas has a head, a body, and a tail. It delivers pancreatic juice to the duodenum through the pancreatic duct. OpenStax |
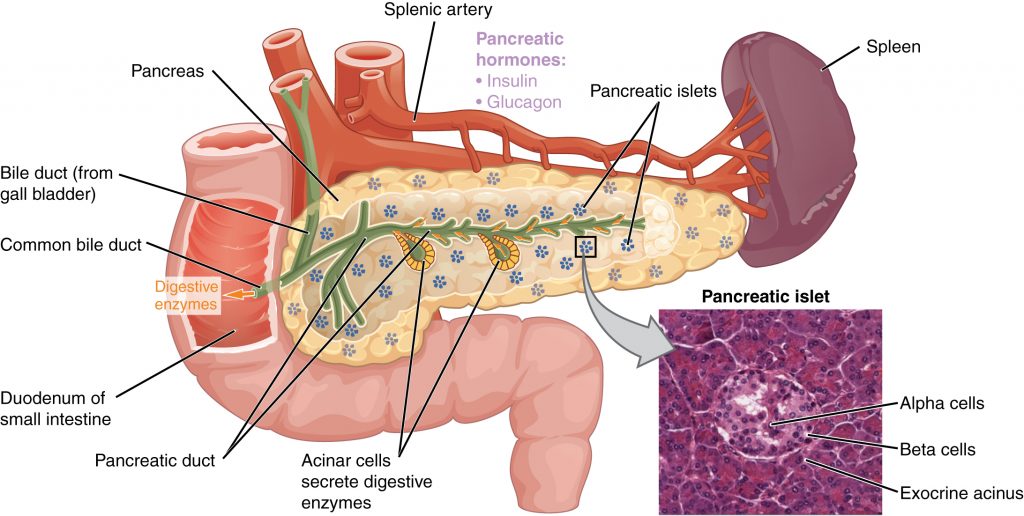 |
| Pancreas The pancreatic exocrine function involves the acinar cells secreting digestive enzymes that are transported into the small intestine by the pancreatic duct. Its endocrine function involves the secretion of insulin (produced by beta cells) and glucagon (produced by alpha cells) within the pancreatic islets. These two hormones regulate the rate of glucose metabolism in the body. The micrograph reveals pancreatic islets. LM × 760. (Micrograph provided by the Regents of University of Michigan Medical School © 2012) |
Figure 23.18: Pancreas
Histological organization of the pancreas
The pancreas serves as both an exocrine (releases product through a duct) and endocrine (releases hormones in the bloodstream) organ. Most of the cells of the pancreas are devoted to its exocrine function. Simple cuboidal cells are arranged in pockets known as pancreatic acini. This grouping of cells produces — a collection of water, digestive enzymes, and bicarbonate to help neutralize the acidic chyme from the stomach. The digestive enzymes accelerate the chemical breakdown of substances that have moved from the stomach to the duodenum. Scattered throughout the pancreatic acini are pancreatic islets (islets of Langerhans) which produce hormones involved with blood glucose regulation. The endocrine function of the pancreas is discussed in the endocrine system chapter [link to endocrine system section about the pancreas/insulin].
Physiology of the Pancreas
Recall that chyme from the stomach can be very acidic. When it enters the duodenum, the low pH triggers the release of the hormone secretin while protein and lipids trigger the release of choleocystokinin (CCK). Secretin in turn triggers the release of bicarb-rich juice from the pancreas and liver. This alkaline secretion acts to increase the pH of the chyme in the duodenum protecting its delicate mucosa layer. CCK triggers the contraction of the gallbladder, the relaxation of the hepatopancreatic sphincter, and the release of pancreatic enzymes from the pancreas to accelerate the chemical breakdown of foodstuffs. The pancreatic enzymes consist of carbohydrases, lipases, nucleases, and proteases that accelerate the chemical breakdown of carbohydrates, lipids, nucleic acids, and proteins respectively.
23.9 Small Intestine
![]() 23.9 Learning Outcomes
23.9 Learning Outcomes
By the end of this section, you will be able to:
- Compare and contrast the location and gross anatomy of the small intestine
- Describe how unique arrangements of the small intestine wall increase its absorptive capacity
- Describe the mechanical and chemical digestion of chyme upon its release into the small intestine
The small intestine is the longest part of the GI tract and one of its main functions is to complete digestion and absorb nutrients, water, vitamins, and minerals from the food you ingest.
Gross Anatomy of the Small Intestine
The small intestine receives partially digested chyme from the stomach and is the next segment of the gastrointestinal tract. The small intestine is a long 4.5 to 7.5 m (14.8 to 24.6 ft) tube-like structure where chemical digestion tries to break down digested food into molecules small enough to be absorbed by the epithelial cells along its length. Even though the small intestine is much longer than your height, it manages to fit in your body by a series of turns that wind and tightly coil the intestines in your abdomen.
There are three main regions of the small intestine that chyme eventually travels through on its way to the large intestine. In order, these are the duodenum, , and . The ileum ends at a sphincter called the ileocecal valve that leads to the of the large intestine.
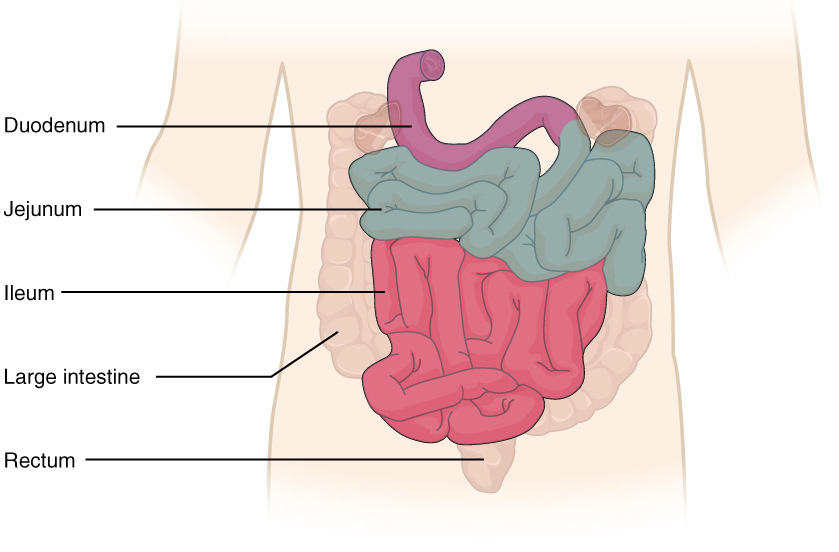
Figure 23.19: Small Intestine [OpenStax]
Histology of the Small intestine
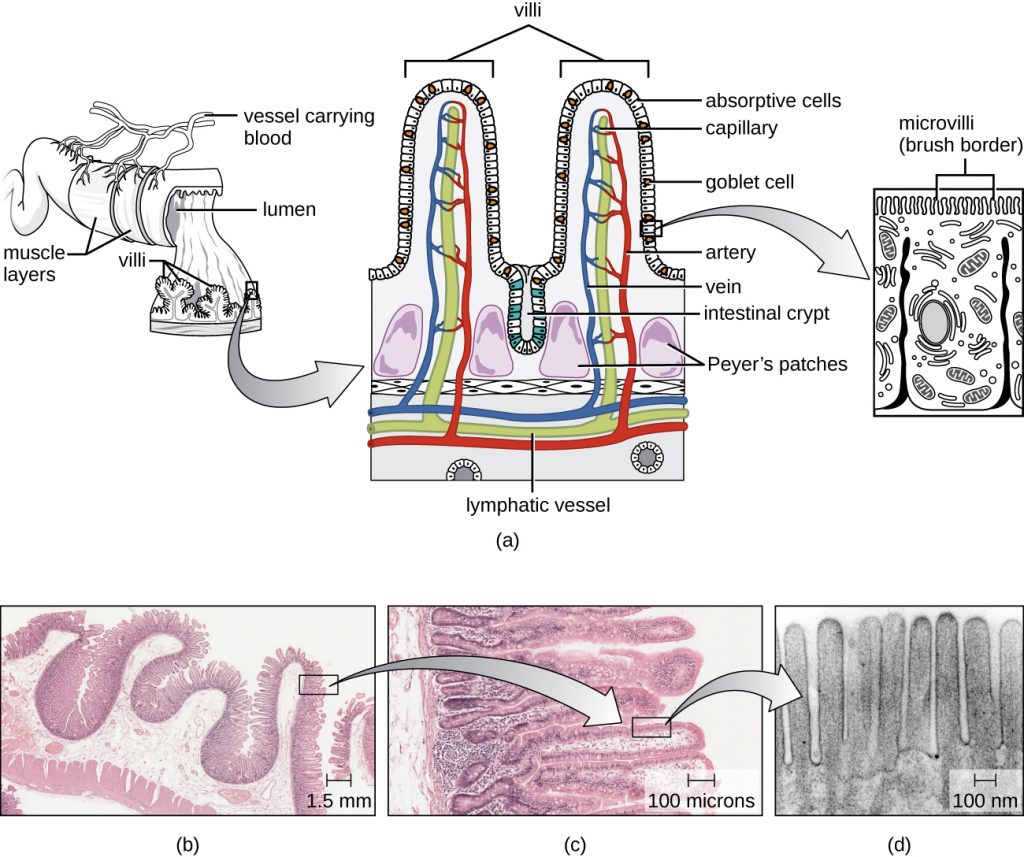 |
| Histology of the Small Intestine: (a) The structure of the wall of the small intestine allows for the majority of nutrient absorption in the body. (b) Villi are folds in the surface of the small intestine. Microvilli are cytoplasmic extensions on individual cells that increase the surface area for absorption. (c) A light micrograph shows the shape of the villi. (d) An electron micrograph shows the shape of the microvilli. (credit b, c, d: Modification of micrographs provided by the Regents of University of Michigan Medical School © 2012) |
 |
| Transmission electron microscope image of a thin section cut through an epithelial cell from a human jejunum (segment of the small intestine). The image shows the apical end of an absorptive cell with some of the densely packed microvilli that make up the striated border. Each microvillus is approximately 1 μm long by 0.1 μm in diameter and contains a core of actin microfilaments. (credit: “Microvilli”, Wikimedia Commons) [From OpenStax Bio AP] |
Figure 23.20: Layers of the small intestine
The layers of the wall of the small intestine are continuous with the mucosa, submucosa, muscular layer, and serosa of the stomach. However, the mucosa of the small intestine takes on a much different shape than the rugae of the stomach. The small intestine has many s (also called plicae circulares) that appear like ruffles lining its inner surface. The circular folds are oriented perpendicular to the path of chyme traveling through the small intestine which helps to slow the passage giving enzymes the extra time needed to break down the macromolecules into smaller molecules that can be absorbed. These circular folds also drastically increase the total inner surface area of the small intestines to increase the efficiency of absorption of nutrients, water, minerals, and vitamins from digested food.
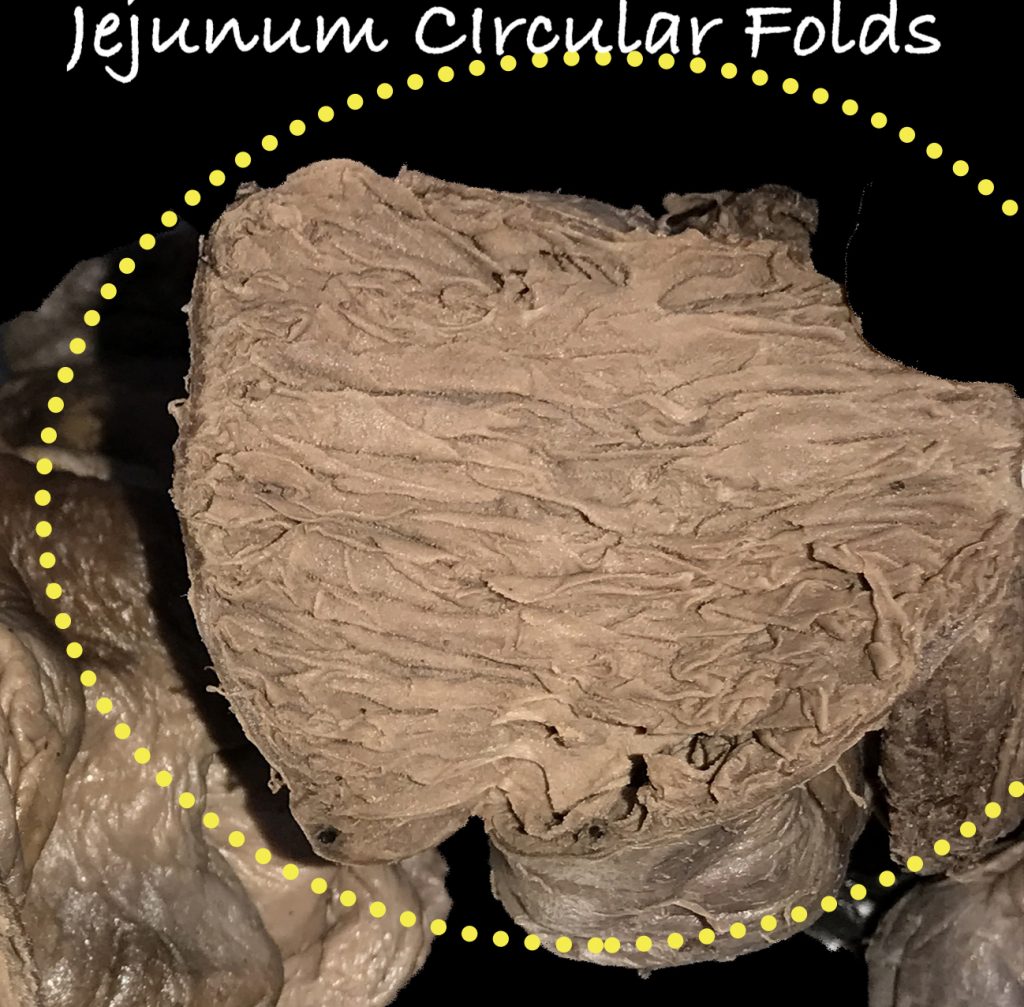
Figure 23.21: Circular folds
The circular folds are covered by a dense carpet of intestinal villi (singular ), which are small (0.5 to 1 mm long) finger-like projections that help to further increase the inner surface area of the small intestine, and there are about 20 to 40 villi per square millimeter.
The epithelial cells on the surface of each villus are also covered with even smaller (~1 µm) projections called microvilli (singular ) on their apical surface, which exponentially increase the surface area of the small intestine for yet even more absorption of nutrients. The layer of microvilli on the surface of these epithelial cells are so fine that they are sometimes called a since they project from the cells like bristles on a paintbrush. There are many brush border enzymes on the surface of the microvilli that help to further digest carbohydrates and proteins into even smaller molecules that can be absorbed through the epithelial cells of the small intestine. , , and , are examples of brush border enzymes that break down disaccharides into monosaccharides. There are also a wide variety of peptidases that help to break down peptides into amino acids, and lipases that help to break down triglycerides into free fatty acids, monoglycerides, and glycerol. A deficiency in one or more of these enzymes can cause problems with digestion, such as bloating and diarrhea experienced by people who are lactase-deficient (commonly called lactose intolerance) when they eat foods containing large amounts of lactose such as dairy products.
![]() Retrieval Practice
Retrieval Practice
Digestive Enzymes of the Mouth, Stomach, Pancreas, and Small Intestine
Without looking at your book or notes, make a list of all the enzymes of the mouth, stomach, pancreas, and small intestine. Along with their names, include their function and any notable details you can recall from the textbook. When your document is complete, check your work and make corrections and additions.
The villi also have an internal structure supported by the lamina propria layer that provides a scaffold for nerves and many vessels that transport nutrients absorbed from the intestinal epithelium. There are small capillary beds within each villus that pick up water-soluble nutrients and molecules such as carbohydrates, amino acids, and some vitamins and transport them in the blood that circulates to and from the villi. Blood flowing from the villi eventually leads to the hepatic portal vein that leads to the liver, and then to systemic circulation. Within the villi, there are also vessels called lacteals, which are different from the capillaries, and are a special type of lymphatic capillary. These lacteals serve as an alternate route for lipids and fats absorbed by the digestive system, instead of fats directly entering blood capillaries. The fats absorbed by lacteals instead enter the lymphatic system, bypassing the hepatic portal circulation, and eventually are returned to the systemic circulation via the cisterna chyli and then the thoracic duct.
In addition to the numerous circular folds, villi, and microvilli lining the intestines, the mucosa of the intestine contains sunken crevices that lead to tubular s (also called intestinal crypts or crypts of Lieberkühn) at the bottom of these crevices. Intestinal glands produce a watery, slightly alkaline secretion called , which is mostly a mixture of water and mucus along with some enzymes. In addition, enteroendocrine cells within the intestinal glands secrete hormones into the blood. Approximately 0.95 to 1.9 liters of intestinal juice are secreted daily, and the enzymes and molecules found in intestinal juice help to neutralize acidic chyme coming from the stomach and activate digestive enzymes. The small intestine may increase secretion of intestinal juice in response to stretch and distention, the presence of nutrients, or irritating stimuli such as the acidic pH of chyme. These same stimuli cause the enteroendocrine cells to secrete hormones such as gastrin, CCK, and secretin.
The Duodenum
The duodenum is the shortest region 25.4 cm (10 in) of the small intestine, but it serves the important function of being the first part of the small intestine to process chyme arriving from the stomach. The hook-shaped C-curvature of the duodenum cradles the head and length of the pancreas, which also aids in the functioning of digestion that occurs in the duodenum. The duodenum has four segments: superior, descending, horizontal, and ascending. The duodenum ends at a bend called the duodenojejunal flexure, where it becomes the jejunum.
As mentioned in other sections of this chapter, in addition to receiving chyme from the stomach, the duodenum receives secretions such as bile and pancreatic juices from the liver and pancreas, respectively. Some refer to the duodenum as the “mixing bowl”. The bile from the liver helps to break apart and emulsify fats found in chyme. Pancreatic juice contains a wide variety of enzymes that help to break down macromolecules and its alkaline properties help to neutralize the highly acidic pH of chyme. The bile duct and merge at a structure called the (also called the ampulla of Vater). The hepatopancreatic ampulla combines bile and pancreatic juice and secretes them into the duodenum via a small volcano-shaped . The release of these secretions can be further controlled by the hepatopancreatic sphincter (also called the sphincter of Oddi), which contracts and relaxes to regulate the flow of bile and pancreatic juice.
Although a major function of the duodenum is to mix chyme with digestive secretions, the duodenum is less specialized for the absorption of nutrients. Accordingly, form follows function. There are very few circular folds and smaller villi that cover the inside surface of the duodenum as compared to the other regions of the small intestine. The duodenum also has numerous submucosal s (also called Brunner’s glands) that produce alkaline secretions that help to neutralize the very acidic pH of chyme and eventually bring the pH back up to around 7-8. These secretions help to protect the duodenum and downstream segments of the intestines from the chemical properties of chyme as it exits the stomach.
The duodenum is also important in secreting a wide variety of hormones that affect digestive functions. When chyme enters the duodenum, the low pH causes the enteroendocrine cells to secrete a peptide hormone called secretin which has many functions and targets in the body. One of the main functions of secretin is to target the pancreas and increase the production of alkaline bicarbonate buffers by the pancreas, which helps to further neutralize and increase the pH of chyme. Secretin also stimulates bile production by the liver which further aids in digesting chyme. Secretin also provides feedback to the stomach which reduces gastric motility and secretions by the stomach.
Cholecystokinin (CCK) is a peptide hormone produced by the enteroendocrine cells in the duodenal glands in response to chyme, especially when the chyme is rich in fats and proteins. For example, having breakfast with a lot of spam and Portuguese sausage may increase your duodenal production of CCK compared to eating a bagel.
CCK stimulates the pancreas to increase the secretion of all pancreatic digestive enzymes. CCK also stimulates the gallbladder to contract and eject more bile and relaxes the hepatopancreatic sphincter to increase the flow of bile and pancreatic juice into the duodenum. CCK also provides feedback to the stomach which decreases gastric motility and secretion and acts on CCK receptors in the nervous system that suppresses hunger and increases satiety.
Gastric inhibitory peptide (GIP) is a hormone produced by the duodenum, and true to its name, GIP provides feedback to the stomach and inhibits gastric motility and emptying. GIP is produced in response to fats and carbohydrates, and one of its other functions is to stimulate the production of insulin by the pancreas in response to the presence of carbohydrates. GIP also has many secondary effects, including stimulating duodenal gland activity, lipid synthesis, and glucose metabolism.
The duodenum also produces other hormones such as gastrin (also produced by the stomach); vasoactive intestinal peptide, which stimulates intestinal gland secretion and affects intestinal blood flow by dilating arterioles; and enterocrinin, which stimulates alkaline mucus production by intestinal glands.
| Hormone or peptide | Molecular weight (Da) | Number of amino acids | Main gut localization | Principal physiologic actions |
|---|---|---|---|---|
| Gastrin family | ||||
| Cholecystokinin | 3918 | 33 (also 385, 59) | Duodenum and jejunum, Enteric nerves | Stimulates gallbladder contraction and intestinal motility; stimulates secretion of pancreatic enzymes, insulin, glucagon, and pancreatic polypeptides; has a role in indicating satiety; the C-terminal 8 amino acid peptide cholecystokinin (CCK)-8 retains full activity |
| Little gastrin | 2098 | 17 | Both forms of gastrin are found in the gastric antrum and duodenum | Gastrins stimulate the secretion of gastric acid, pepsinogen, intrinsic factor, and secretin; stimulate intestinal mucosal growth; increase gastric and intestinal motility |
| Big gastrin | 3839 | 34 | ||
| Secretin-glucagon family | ||||
| Secretin | 3056 | 27 | Duodenum and jejunum | Stimulates pancreatic secretion of HCO3, enzymes and insulin; reduces gastric and duodenal motility, inhibits gastrin release and gastric acid secretion |
| Vasoactive intestinal polypeptide (VIP) | 3326 | 28 | Enteric nerves | Relaxes smooth muscle of gut, blood vessels, and genitourinary system; increases water and electrolyte secretion from pancreas and gut; releases hormones from pancreas, gut, and hypothalamus |
| Glucose-dependent insulinotropic | 4976 | 42 | Duodenum and jejunum | Stimulates insulin release; reduces gastric and intestinal motility; increases fluid and electrolyte secretion from small intestine |
| Hormone or peptide | Major tissue locations in the gut | Principal known actions |
|---|---|---|
| Bombesin | Throughout the gut and pancreas | Stimulates release of cholecystokinin (CCK) and gastrin |
| Calcitonin gene-related peptide | Enteric nerves | Unclear |
| Chromogranin A | Neuroendocrine cells | Secretory protein |
| Enkephalins | Stomach, duodenum | Opiate-like actions |
| Enteroglucagon | Small intestine, pancreas | Inhibits insulin secretion |
| Galanin | Enteric nerves | |
| Ghrelin | Stomach | Stimulates appetite, increases gastric emptying |
| Glucagon-like peptide 1 | Pancreas, ileum | Increases insulin secretion |
| Glucagon-like peptide 2 | Ileum, colon | Enterocyte-specific growth hormone |
| Growth factors | Throughout the gut | Cell proliferation and differentiation |
| Growth hormone-releasing factor | Small intestine | Unclear |
| Leptin | Stomach | Appetite control |
| Motilin | Throughout the gut | Increases gastric emptying and small bowel motility |
| Neuropeptide Y | Enteric nerves | Regulation of intestinal blood flow |
| Neurotensin | Ileum | Affects gut motility; increases jejunal and ileal fluid secretion |
| Pancreatic polypeptide | Pancreas | Inhibits pancreatic and biliary secretion |
| Peptide YY | Colon | Inhibits food intake |
| Somatostatin | Stomach, pancreas | Inhibits secretion and action of many hormones |
| Substance P | Enteric nerves | Unclear |
| Trefoil peptides | Stomach, intestine | Mucosal protection and repair |
Table 23.1 : Summary of intestinal hormones
The Jejunum
The duodenum becomes the jejunum after a bend called the duodenojejunal flexure, which is anchored by a thin muscle that supports and suspends that bend. At the flexure, the jejunum also enters back into the peritoneal cavity and is supported by a sheet of mesentery. The jejunum has an average length of about 2.5m (8.2 ft) and is about two-fifths of the overall length of the small intestines and is generally located in the left superior part of the peritoneal cavity.
Features such as circular folds and villi are more prominent and numerous at the proximal end (toward the duodenal side) of the jejunum. As mentioned earlier in this chapter, these features increase surface area and absorption, which is one of the main functions of the jejunum. Most nutrient absorption in the intestine occurs in the jejunum before chyme enters the ileum. In line with this, more nutrient absorption occurs at the proximal end of the jejunum, and as the jejunum transitions to become the ileum, the circular folds and villi gradually decrease in size.
The Ileum
The ileum is the next intestinal region after the jejunum and is the longest and final segment of the small intestine with an average length of about 3.5 m (11.5 ft), which is about three-fifths of the total length of the small intestine. There is no clear physical landmark or border that separates the jejunum from the ileum on the GI tract itself. Despite the lack of a visible border, there are general differences such as the ileum being generally located in the right inferior part of the peritoneal cavity, the walls are thinner in the ileum than the jejunum, and the circular folds of the ileum are thinner and less prominent than those in the jejunum. The distal part of the ileum next to the cecum lacks circular folds altogether.
The ileum is also supported by mesentery and there are subtle differences between the mesenteries of the ileum and jejunum. Generally, the mesentery of the ileum has more fat and the vasculature between the mesenteries of the ileum and jejunum also have different arrangements.
Compared with the duodenum and jejunum, the ileum also contains numerous collections of lymphoid tissue called aggregated lymphoid nodules (also called Peyer’s patches). Aggregated lymphoid nodules appear as round or oval-shaped bumps within the mucosa and extend into the submucosa of the ileum, and are most numerous in the distal part of the ileum next to the cecum of the large intestine. Lymphocytes located in these nodules protect the small intestine from bacteria that are naturally present in the large intestine.
Digestion and Absorption in the Small Intestine
The small intestine moves chyme along its length differently from how the esophagus and stomach move and mix food. The small intestine contracts using a form of peristalsis called es. These complexes cause the small intestine to contract differently from the peristalsis seen in the esophagus. Instead of sensing a mass of digested food and squeezing it toward the next organ, sections of the small intestine alternate and take turns in contracting. This results in a form of movement called segmentation, in which chyme moves back and forth along the length of the small intestine instead of heading in only one direction toward the next intestinal region. This backtracking allows the contents of each segment to mix and lengthens the time that chyme spends in the small intestine, thus giving more time for digestion and absorption of nutrients from chyme.
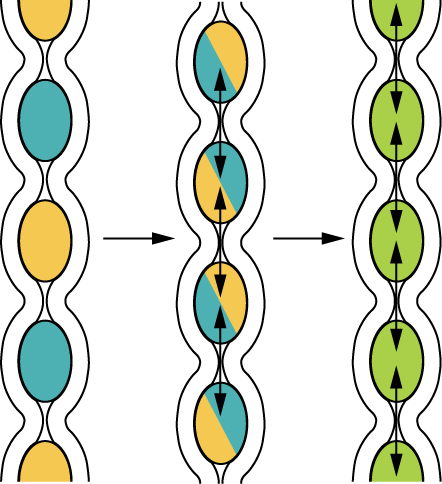
Figure 23.22: Segmentation: Segmentation separates chyme and then pushes it back together, mixing it and providing time for digestion and absorption. [From OpenStax]
Segmentation and migrating motility complexes also help to further mix chyme with emulsifiers found in bile and the enzymes found in pancreatic juice and preceding parts of the GI tract. The increased time that chyme spends in the small intestine due to its back-and-forth movement also means longer exposure and more digestion by brush border enzymes, which help to further break down any remaining macromolecules into smaller nutrients that can be absorbed by the intestinal epithelium.
![]() Food and Environment
Food and Environment
Juicy Tropical Fruits
The small intestine is important in reabsorbing water from the GI tract, with approximately 90% of the food and beverages you ingest being absorbed into the walls of the small intestine. This absorption allows your body to obtain both nutrition and hydration by eating juicy fruits like mangoes, papayas, and bananas, or foods with a lot of water content like poi.

Figure 23.23: Plate of ʻono mango
In summary, the overall function of the small intestine is to promote nutrient and water absorption. Nutrient and water absorption are promoted by various factors provided by the small intestine. The small intestine provides for the combination of enhanced surface area, chemical digestion, time, mixing, and exposure to pancreatic and intestinal enzymes to perform its critical function.
23.10 Large Intestine
![]() 23.10 Learning Outcomes
23.10 Learning Outcomes
By the end of this section, you will be able to:
- Compare and contrast the location and gross anatomy of the large intestine
- Identify the beneficial roles of the in the digestive system functioning
- List three features unique to the wall of the large intestine and identify their contributions to their function
- Trace the pathway of food waste from its point of entry into the large intestine through its exit from the body as feces
Gross Anatomy of the Large Intestine
The large intestine is the next segment of the GI tract after the small intestine terminates at the ileum. Even though the large intestine has an average length of 1.5 meters (5 ft) when stretched out, it is shorter in length than the small intestine. The large intestine is called “large” because it appears thicker with an average diameter is 7.5 cm (3 in), which is more than twice the average diameter of the small intestines.
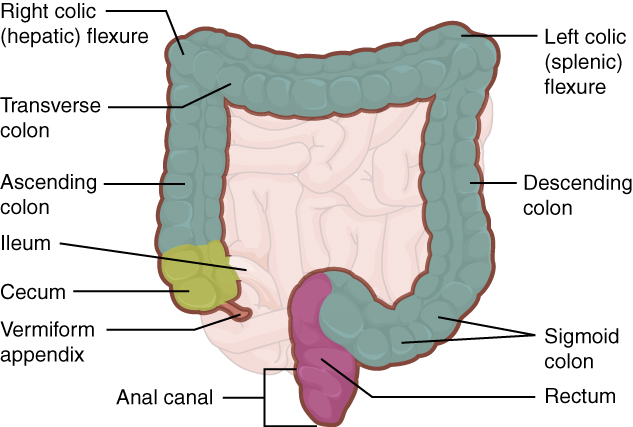
Figure 23.24: Large intestine [from OpenStax]
The large intestine is arranged in a loop that frames the small intestine at its lateral and superior borders. There are three main segments of the large intestine: the cecum, colon, and rectum.
Three features are unique to the large intestine: teniae coli, haustra, and s. The teniae coli are three bands of smooth muscle that are made up of the longitudinal muscle layer of the muscularis of the large intestine, except at its terminal end. Tonic contractions of the teniae coli bunch up the colon into a succession of pouches called haustra (singular = ), which are responsible for the wrinkled appearance of the colon. Attached to the teniae coli are small, fat-filled sacs of visceral peritoneum called epiploic appendages. The purpose of these is unknown. Although the rectum and have neither teniae coli nor haustra, they do have well-developed layers of muscularis that create the strong contractions needed for defecation.
The Cecum
The cecum is the first part of the large intestine and colon that receives digested food from the small intestine and is shaped like a pouch that is about 6 cm (2.4 in) long. The cecum is joined to the ileum by the ileocecal valve, which transfers the contents of the cecum to the ileum. Instead of absorbing nutrients like the small intestine, the cecum continues the process of absorbing water and salts from digested food and begins the process of compacting (eliminating water) undigested materials into waste.
The (also, vermiform appendix) is a slender tube that emerges from the tip of the cecum and has an average length of 9 cm (3.5 in). However, its size and shape vary widely and can range from 5 to 35 cm in length (2 to 13.7 in). The appendix has a mesentery called the that anchors it to the ileum and cecum.
The appendix contains lymphoid tissue, but as of this writing, its exact role in the immune system is still being researched. Appendicitis is an inflammation of the appendix that is often painful and can be potentially fatal if the appendix ruptures or bursts, which leaks bacteria found inside the large intestine into the abdominal cavity. Appendicitis is typically treated with surgical removal (appendectomy) and antibiotics. Fortunately, people can live normal healthy lives after an appendectomy.
The appendix and cecum in many animals are larger relative to that of humans. As a result, it was previously thought that the appendix in humans is a vestigial organ, meaning that it has reduced in size and function during human evolution. However, this view has been challenged by recent discoveries about gut immunity and bacteria that are normally found in our large intestines. One theory is that the appendix serves as a “storehouse” for microorganisms that are normally found in our large intestine and are beneficial to our health. One hypothesis from this theory is that when something wipes out the population of microbes normally found in our gut (for example, diarrhea), the microbes stored in the appendix help with reestablishing and repopulating the gut with those microbes.
The Colon
The cecum continues to the rest of the colon, which frames the small intestine along the lateral and superior borders of the small intestine, and part of the inferior border. The colon itself is divided into segments according to how it travels through the abdomen. When fecal matter first leaves the cecum, it travels upwards along the , in which food residue moves superiorly on the right side of the abdomen. The colon then makes a sharp bend called the (also, hepatic flexure) and then becomes the , which travels horizontally along the transverse plane toward the left side of the body. The colon then makes another sharp turn called the (also, splenic flexure), where it veers downwards and becomes the , which travels inferiorly along the left side of the body. After the colon enters the pelvic inlet, it becomes the , named after its curvy paths like the letter ‘s’ or the Greek lowercase letter sigma (ς). The sigmoid colon eventually moves toward the midline, where it makes a downward turn and becomes the rectum. Sometimes small abnormal pouches form in the wall of the colon. This is called diverticulosis and becomes increasingly common as we age. Diverticulosis is a painless condition. However, when these pouches become impacted and inflamed it causes an extremely painful condition called diverticulitis. Diverticulitis is most common in the sigmoid colon and is therefore experienced as pain in the lower left quadrant. Frequently, surgeons elect to perform colonic resections of the sigmoid colon to treat the condition.
The segments of the colon are supported by mesenteries and weave in and out of the peritoneal space. The ascending colon, descending colon, and rectum are located retroperitoneally. The transverse and sigmoid colon are tethered to the posterior abdominal wall by the mesocolon.
Colorectal cancer is the third most common and second deadliest type of cancer for both sexes. In colon cancers, tumors develop in the walls of the colon and may require surgical removal, in which surgeons may perform a colon resection to remove part of a segment or entire segments of the colon to remove any tumors and some surrounding tissue in case the cancer has spread further than originally thought. Colon resections may extend the life of someone who has colon cancer, but also has risks due to the chance of infection and disrupting the vast network of blood vessels that supply the colon and surrounding tissues. Surgical teams will do everything to ensure that the reconnected colon does not leak, which is extremely dangerous as it would spill undigested fecal matter and bacteria outside of the colon and into the abdominal cavity.
The Rectum
After food residue leaves the sigmoid colon, it enters the rectum, the final segment of the GI tract. The rectum is located in the pelvis and is about 20 cm (8 in) in length on average. The rectum travels downward in the pelvis and bends to extend anteriorly and follow the curvature of the sacrum and coccyx. The rectum also has three lateral bends that create a series of internal transverse folds called s. These valves help separate feces from gas to prevent the simultaneous passage of feces and gas.
The anal canal is the final 4 to 5 cm (1.5 to 2 in) long part of the rectum that begins when the rectum exits the abdominopelvic cavity and ends at the anus. As chyme travels through the large intestine, most of the remaining water is removed and the undigested materials are compressed and compacted. This process eventually converts residual chyme into semi-solid feces (also, stool). Feces is a mixture of a variety of materials, including undigested food, unabsorbed substances, mucus, bacteria, epithelial cells sloughed off from GI mucosa, salts, and enough water to let feces travel smoothly out of the body. The anal canal includes two rings of muscle called sphincters, which control the release of feces from the body. The sphincters of the anal canal are different in their histology and how they are controlled. The is made of smooth muscle, and its contractions are reflexive and under involuntary control. However, the is made of skeletal muscle, which is under voluntary control.
Both the internal and external anal sphincters open during the process of defecation, which moves and releases feces out of the anus and body and into the environment. Otherwise, both sphincters remain closed when not in the process of defecating. Defecation begins when s force feces from the colon into the rectum. The feces stretch and distend the rectal wall, which initiates the defecation reflex. This results in the coordinated relaxation of both anal sphincters to eliminate feces from the rectum. The defecation reflex is mediated by the sacral spinal cord and under parasympathetic control. At the start of the reflex, the sigmoid colon and rectum contract and move feces toward the anal canal and sphincters.
The presence of feces in the anal canal activates receptors that sense pressure and distension. In turn, a signal is sent to the CNS indicating feces is waiting to be released. This signal gives the individual extra time to choose to voluntarily open the external anal sphincter and defecate, or keep the sphincter closed until it is a more appropriate time. If you decide to hold off on defecating, there is a few seconds delay for the reflexive contractions to stop and the rectal walls to relax. The next mass movements will push more feces into the canal and trigger additional defecation reflexes until you eventually defecate.
The Valsalva maneuver is a voluntary procedure that assists in pushing feces from the body by contracting your diaphragm and abdominal wall muscles and closing your glottis. This maneuver increases intra-abdominal pressure which generates additional force to push feces out.
![]() Deep Dive
Deep Dive
Now that you have read about the digestive system, grab a piece of paper and see if you can, by memory, write out all of the GI structures in the order a bite of food will travel through; starting with the mouth and ending with the anus.
Histology of the Large Intestine
The mucosa, submucosa, muscular layer, and serosa of the large intestine are continuous with the small intestine, but there are several key differences between the walls of the large and small intestines. In the walls of the large intestine, there are relatively few enzyme-secreting cells and there are no circular folds or villi. Most of the mucosa of the colon is simple columnar epithelium made mostly of enterocytes (absorptive cells) and goblet cells. In the anal canal, the mucosa becomes thicker and is made up of a variety of epithelia, including simple columnar epithelium which transitions into stratified squamous epithelium at the end of the anal canal. In addition, the wall of the large intestine has far more intestinal glands, which contain a vast population of enterocytes and goblet cells. These goblet cells secrete mucus that lubricates and eases the movement of feces and protects the intestine from the effects of the acids and gasses produced by enteric bacteria. The enterocytes absorb water and salts as well as vitamins produced by your intestinal bacteria.
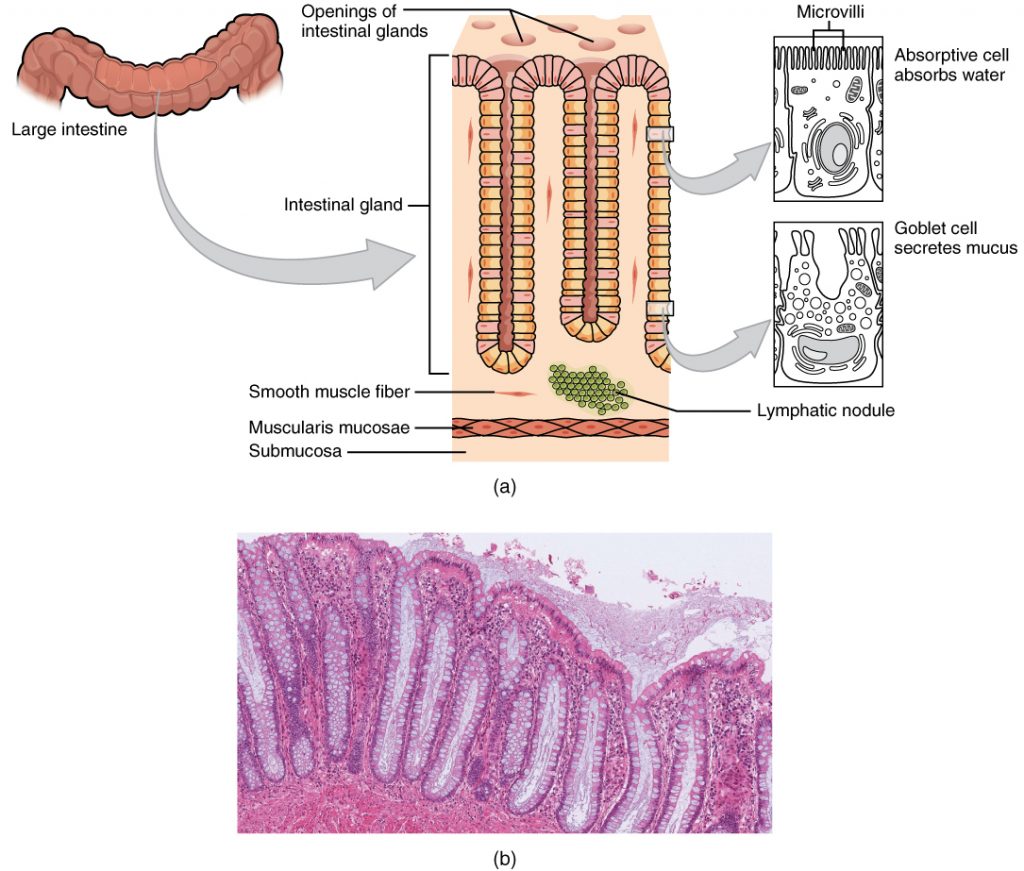
Figure 23.25: Histology of the large Intestine: (a) The histologies of the large intestine and small intestine (not shown) are adapted for the digestive functions of each organ. (b) This micrograph shows the colon’s simple columnar epithelium and goblet cells. LM x 464. (credit b: Micrograph provided by the Regents of University of Michigan Medical School © 2012) [from OpenStax]
The Gut Microbiome
A recent fascinating area of study is the gut microbiome. This refers to the organisms (mainly bacteria) that live in the digestive tract. It is now known that the microorganisms in your GI tract may have a myriad of important impacts on the physical and mental health of an individual. Each person has a unique colony of these microorganisms living in their GI tract and they have been shown to influence a broad range of conditions including an individual’s ability to resist infection, immune function, maintenance of mucosa epithelium in the gut, and even behavior and mental health.
The types of microorganisms vary within different sections of the GI tract. The colon contains the largest number of microbes. Some Intestinal bacteria benefit the host as they are involved with the synthesis of vitamins such as B vitamins and vitamin K, as well as the production of short-chain fatty acids. These short-chain fatty acids, when absorbed, act somewhat like hormones. The disruption of healthy gut flora has been correlated with numerous inflammatory and autoimmune diseases including obesity. Having a healthy population of gut flora is also important in preventing pathogenic bacteria from establishing themselves in the colon and causing disease.
![]() Local Issue
Local Issue
In Native Hawaiian and Pacific Islands cultures, the land was the primary source of both food and medicine. Rather than eating processed foods, Native Hawaiians and other Pacific Islanders relied on the land to feed them and developed complex systems of agriculture, aquaculture, and medicinal herb practices. These systems were disrupted by colonization, displacement from the land, and the introduction of processed foods. Food consumption has been disconnected from the land and food production. Traditional practices of medicinal herbs have also been disrupted. This has resulted in negative health outcomes for NHPI populations, including negative health indicators and intergenerational trauma. Several studies have shown that programs to reconnect NHPI to land and traditional food and medicinal herb practices may lead to a reduction in trauma symptoms and increase positive impacts on overall well-being among these populations. On the UH Mānoa campus, the Loʻi at Kānewai allows students and community members to engage in kalo farming practices and other medicinal herb practices such as learning about ʻawa.
Digestion and Absorption in the Large intestine
When chyme enters the large intestine, there are very few nutrients left and most of the water has been reabsorbed. The large intestine continues to reabsorb water as the residual chyme is compacted and eventually becomes feces.
In the large intestine, mechanical digestion begins when peristalsis moves chyme from the ileum, through the , and into the cecum. When the cecum is distended with chyme, the ileocecal sphincter prevents additional chyme from being added and prevents backward movement of chyme and bacteria from the cecum back into the ileum.
Mechanical digestion in the large intestine includes a combination of three types of movements. The presence of fecal residues in the colon stimulates a slow-moving . This type of movement occurs mostly in the transverse and descending colons and involves sluggish segmentation and contractions of individual pouch-like haustra. When a haustrum is distended with chyme, its muscle contracts and pushes its contents into the next haustrum. Each haustral contraction occurs about every 30 minutes and lasts about 1 minute. These movements also mix the food residue, which helps the large intestine absorb water. The second type of movement is peristalsis, which, in the large intestine, is slower than in the more proximal portions of the alimentary canal. The third type is mass movement. These strong waves start midway through the transverse colon and quickly force the contents toward the rectum. There can be long pauses between mass movements, and these movements usually occur three or four times per day, either while you eat or immediately afterward. Distension in the stomach and the breakdown products of digestion in the small intestine provoke the , which increases motility, including mass movements, in the colon. Fiber in the diet both softens the stool and increases the power of colonic contractions, optimizing the activities of the colon.
The large intestine glands secrete mucus, but they do not secrete digestive enzymes of the kind found in the small intestines. In the large intestine, bacteria in the lumen of the colon play a larger role in chemical digestion than digestive enzymes produced by our own body. is a process in which bacteria break down some of the remaining carbohydrates. The fermentation and gasses produced by the bacteria result in the production of hydrogen, carbon dioxide, and methane gasses that can accumulate and create (gas) in the colon. Flatulence is excessive flatus, and each day, up to 1500 mL of flatus is produced in the colon. More is produced when you eat foods such as a chili dish rich in beans, or dishes that contain a lot of garlic. These foods are rich in otherwise indigestible sugars or complex carbohydrates like soluble dietary fiber, which can be fermented by bacteria in the colon, thus causing increased flatus production and flatulence.
Although the small intestine absorbs the majority of water found in chyme (about 7.8 L per day), the large intestine plays a significant role in helping to conserve and reabsorb more water (about 1.2 L per day). Some water is usually leftover in the residual chyme as it is turned into feces in the colon, otherwise, it would result in hard and dry feces that would be painful to pass through defecation. However, after chyme has passed through both the small and large intestines and turned into feces, it has lost most of its mass and volume. For every 500 mL (17 ounces) of food residue that enters the cecum each day, about 150 mL (5 ounces) become feces.

Chapter Summary
References
- Small intestine:
- https://openstax.org/books/anatomy-and-physiology/pages/23-5-the-small-and-large-intestines
- https://radiopaedia.org/articles/jejunum-vs-ileum-1?lang=us
- Large intestine
- Schumpelick V, Dreuw B, Ophoff K, Prescher A. Appendix and cecum. Embryology, anatomy, and surgical applications. Surg Clin North Am. 2000 Feb;80(1):295-318. https://linkinghub.elsevier.com/retrieve/pii/S0039610905704072
- Anal canal histology: https://pubmed.ncbi.nlm.nih.gov/22718291/
- Na’au
- file:///Users/rromine/Dropbox/UHWO/Anatomy%20learning%20group/Book%20sprint/Resources/Culture/na-au-word-bank-university-of-hawaii.pdf

Key Terms
absorption
passage of digested products from the intestinal lumen through mucosal cells and into the bloodstream or lacteals
accessory digestive organ
includes teeth, tongue, salivary glands, gallbladder, liver, and pancreas
alimentary canal
continuous muscular digestive tube that extends from the mouth to the anus
anal canal
final segment of the large intestine
appendix
(vermiform appendix) coiled tube attached to the cecum
ascending colon
first region of the colon
bacterial flora
bacteria in the large intestine
bile
alkaline solution produced by the liver and important for the emulsification of lipids
bilirubin
main bile pigment, which is responsible for the brown color of feces
body
mid-portion of the stomach
bolus
mass of chewed food
brush border
fuzzy appearance of the small intestinal mucosa created by microvilli
cardia
(also, cardiac region) part of the stomach surrounding the cardiac orifice (esophageal hiatus)
cecum
pouch forming the beginning of the large intestine
central vein
vein that receives blood from hepatic sinusoids
cephalic phase
(also, reflex phase) initial phase of gastric secretion that occurs before food enters the stomach
chemical digestion
enzymatic breakdown of food
chief cell
gastric gland cell that secretes pepsinogen
chyme
soupy liquid created when food is mixed with digestive juices
circular fold
(also, plica circulare) deep fold in the mucosa and submucosa of the small intestine
colon
part of the large intestine between the cecum and the rectum
common bile duct
structure formed by the union of the common hepatic duct and the gallbladder’s cystic duct
crown
portion of tooth visible superior to the gum line
cuspid
(also, canine) pointed tooth used for tearing and shredding food
cystic duct
duct through which bile drains and enters the gallbladderdefecation
elimination of undigested substances from the body in the form of feces
deglutition
three-stage process of swallowing
dentin
bone-like tissue immediately deep to the enamel of the crown or cementum of the root of a tooth
descending colon
part of the colon between the transverse colon and the sigmoid colon
duodenal gland
(also, Brunner’s gland) mucous-secreting gland in the duodenal submucosa
duodenum
first part of the small intestine, which starts at the pyloric sphincter and ends at the jejunum
enamel
covering of the dentin of the crown of a tooth
enteroendocrine cell
gastric gland cell that releases hormones
enterohepatic circulation
recycling mechanism that conserves bile salts
epiploic appendage
small sac of fat-filled visceral peritoneum attached to teniae coli
esophagus
muscular tube that runs from the pharynx to the stomach
external anal sphincter
voluntary skeletal muscle sphincter in the anal canal
feces
semisolid waste product of digestion
flatus
gas in the intestine
fundus
dome-shaped region of the stomach above and to the left of the cardia
G cell
gastrin-secreting enteroendocrine cell
gallbladder
accessory digestive organ that stores and concentrates bile
gastric emptying
process by which mixing waves gradually cause the release of chyme into the duodenum
gastric gland
gland in the stomach mucosal epithelium that produces gastric juice
gastric phase
phase of gastric secretion that begins when food enters the stomach
gastric pit
narrow channel formed by the epithelial lining of the stomach mucosa
gastrin
peptide hormone that stimulates secretion of hydrochloric acid and gut motility
gastrocolic reflex
propulsive movement in the colon activated by the presence of food in the stomach
gingiva
gum
haustral contraction
slow segmentation in the large intestine
haustrum
small pouch in the colon created by tonic contractions of teniae coli
hepatic artery
artery that supplies oxygenated blood to the liver
hepatic lobule
hexagonal-shaped structure composed of hepatocytes that radiate outward from a central vein
hepatic portal vein
vein that supplies deoxygenated nutrient-rich blood to the liver
hepatic vein
vein that drains into the inferior vena cava
hepatocytes
major functional cells of the liver
hepatopancreatic ampulla
(also, ampulla of Vater) bulb-like point in the wall of the duodenum where the bile duct and main pancreatic duct unite
hepatopancreatic sphincter
(also, sphincter of Oddi) sphincter regulating the flow of bile and pancreatic juice into the duodenum
hydrochloric acid (HCl)
digestive acid secreted by parietal cells in the stomach
ileocecal sphincter
sphincter located where the small intestine joins with the large intestine
ileum
end of the small intestine between the jejunum and the large intestine
incisor
midline, chisel-shaped tooth used for cutting into food
ingestion
taking food into the GI tract through the mouth
internal anal sphincter
involuntary smooth muscle sphincter in the anal canal
intestinal gland
(also, crypt of Lieberkühn) gland in the small intestinal mucosa that secretes intestinal juice
intestinal juice
mixture of water and mucus that helps absorb nutrients from chyme
intrinsic factor
glycoprotein required for vitamin B12 absorption in the small intestine
jejunum
middle part of the small intestine between the duodenum and the ileum
lactase
brush border enzyme that breaks down lactose into glucose and galactose
lacteal
lymphatic capillary in the villi
large intestine
terminal portion of the alimentary canal
laryngopharynx
part of the pharynx that functions in respiration and digestion
left colic flexure
(also, splenic flexure) point where the transverse colon curves below the inferior end of the spleen
lingual frenulum
mucous membrane fold that attaches the bottom of the tongue to the floor of the mouth
lingual lipase
digestive enzyme from glands in the tongue that acts on triglycerides
liver
largest gland in the body whose main digestive function is the production of bile
lower esophageal sphincter
smooth muscle sphincter that regulates food movement from the esophagus to the stomach
main pancreatic duct
(also, duct of Wirsung) duct through which pancreatic juice drains from the pancreas
major duodenal papilla
point at which the hepatopancreatic ampulla opens into the duodenum
maltase
brush border enzyme that breaks down maltose and maltotriose into two and three molecules of glucose, respectively
mass movement
long, slow, peristaltic wave in the large intestine
mastication
chewing
mechanical digestion
chewing, mixing, and segmentation that prepares food for chemical digestion
mesoappendix
mesentery of the appendix
microvillus
small projection of the plasma membrane of the absorptive cells of the small intestinal mucosa
migrating motility complex
form of peristalsis in the small intestine
molar
tooth used for crushing and grinding food
motility
movement of food through the GI tract
mucosa
innermost lining of the alimentary canal
muscularis
muscle (skeletal or smooth) layer of the alimentary canal wall
myenteric plexus
(plexus of Auerbach) major nerve supply to alimentary canal wall; controls motility
oral cavity
(also, buccal cavity) mouth
oropharynx
part of the pharynx continuous with the oral cavity that functions in respiration and digestion
pancreas
accessory digestive organ that secretes pancreatic juice
pancreatic juice
secretion of the pancreas containing digestive enzymes and bicarbonate
pancreatic lipase
enzyme secreted by the pancreas that participates in lipid digestion
parietal cell
gastric gland cell that secretes hydrochloric acid and intrinsic factor
pepsinogen
inactive form of pepsin
peristalsis
muscular contractions and relaxations that propel food through the GI tract
pharynx
throat
propulsion
voluntary process of swallowing and the involuntary process of peristalsis that moves food through the digestive tract
pulp cavity
deepest portion of a tooth, containing nerve endings and blood vessels
pyloric sphincter
sphincter that controls stomach emptying
pylorus
lower, funnel-shaped part of the stomach that is continuous with the duodenum
rectal valve
one of three transverse folds in the rectum where feces is separated from flatus
rectum
part of the large intestine between the sigmoid colon and anal canal
retroperitoneal
located posterior to the peritoneum
right colic flexure
(also, hepatic flexure) point, at the inferior surface of the liver, where the ascending colon turns abruptly to the left
root
portion of a tooth embedded in the alveolar processes beneath the gum line
ruga
fold of alimentary canal mucosa and submucosa in the empty stomach and other organs
saccharolytic fermentation
anaerobic decomposition of carbohydrates
saliva
aqueous solution of proteins and ions secreted into the mouth by the salivary glands
salivary amylase
digestive enzyme in saliva that acts on starch
salivary gland
an exocrine gland that secretes a digestive fluid called saliva
segmentation
alternating contractions and relaxations of non-adjacent segments of the intestine that move food forward and backward, breaking it apart and mixing it with digestive juices
serosa
outermost layer of the alimentary canal wall present in regions within the abdominal cavity
sigmoid colon
end portion of the colon, which terminates at the rectum
small intestine
section of the alimentary canal where most digestion and absorption occurs
stomach
alimentary canal organ that contributes to chemical and mechanical digestion of food from the esophagus before releasing it, as chyme, to the small intestine
submucosa
layer of dense connective tissue in the alimentary canal wall that binds the overlying mucosa to the underlying muscularis
submucosal plexus
(plexus of Meissner) nerve supply that regulates activity of glands and smooth muscle
sucrase
brush border enzyme that breaks down sucrose into glucose and fructose
tongue
accessory digestive organ of the mouth, the bulk of which is composed of skeletal muscle
transverse colon
part of the colon between the ascending colon and the descending colon
upper esophageal sphincter
skeletal muscle sphincter that regulates food movement from the pharynx to the esophagus
villus
projection of the mucosa of the small intestine
Media Attributions
- olelo_noeau
- Plate Lunch and Haupia: Plate Lunch © CiXeL is licensed under a Public Domain license
- Plate Lunch and Haupia: Haupia © Arnold Gatilao from Fremont, CA, USA is licensed under a CC BY (Attribution) license
- ʻOno SPAM Musubi © Nesnad is licensed under a CC BY (Attribution) license
- Bowl of poi © Bshams is licensed under a Public Domain license
- Poi and Laulau: Laulau © arnold | inuyaki is licensed under a CC BY (Attribution) license
- Components of the Digestive System © OpenStax is licensed under a CC BY (Attribution) license
- Superior and Inferior Mesenteric Arteries. Layers of the Alimentary Canal © OpenStax is licensed under a CC BY (Attribution) license
- Mesenteries: Mesentery © SUM1 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Mesenteries: Side View © Posible2006 adapted by LynleyShimat Lys - English Terms Added is licensed under a CC BY-SA (Attribution ShareAlike) license
- Peristalsis: Peristalsis © OpenStax is licensed under a CC BY (Attribution) license
- Peristalsis: Peristaltic Movements © OpenStax is licensed under a CC BY (Attribution) license
- Mouth, Oral cavity anterior and lateral view: Anterior © OpenStax is licensed under a CC BY (Attribution) license
- Mouth, Oral cavity anterior and lateral view: Lateral © OpenStax is licensed under a CC BY (Attribution) license
- Salivary glands © OpenStax is licensed under a CC BY (Attribution) license
- The Structure of the Tooth © OpenStax is licensed under a CC BY (Attribution) license
- Permanent and Deciduous Teeth © OpenStax is licensed under a CC BY (Attribution) license
- Pharynx © OpenStax is licensed under a CC BY (Attribution) license
- Upper Airway © OpenStax is licensed under a CC BY (Attribution) license
- Esophagus © OpenStax is licensed under a CC BY (Attribution) license
- Esophagus: Layers of Esophageal Wall © https://training.seer.cancer.gov/ugi/anatomy/layers.html is licensed under a Public Domain license
- Esophagus: Esophagus Histology © Guido Fregapani is licensed under a CC BY-SA (Attribution ShareAlike) license
- Esophageal Layers © Boumphreyfr is licensed under a CC BY-SA (Attribution ShareAlike) license
- Stomach © OpenStax is licensed under a CC BY (Attribution) license
- Gastric Gland / Pit © OpenStax is licensed under a CC BY (Attribution) license
- Parietal cell secreting HCL: Parietal cell secretion © Boumphreyfr is licensed under a CC BY-SA (Attribution ShareAlike) license
- Parietal cell secreting HCL: Parietal cell chemistry © Moon rabbit 365 adapted by LynletShimat Lys - English Labels is licensed under a CC BY-SA (Attribution ShareAlike) license
- Parietal cell secreting HCL: Mechanism of the gastric H+/K+ ATPase within parietal cells © Keministi is licensed under a Public Domain license
- The Liver: Accessory Organs © OpenStax is licensed under a CC BY (Attribution) license
- The Liver: The Liver © BruceBlaus is licensed under a CC BY-SA (Attribution ShareAlike) license
- The Liver: Diagram of liver, blood vessels, hepatic lobule, and portal tract anatomy © Gwilz is licensed under a CC BY-SA (Attribution ShareAlike) license
- Gallbladder © OpenStax is licensed under a CC BY (Attribution) license
- Pancreas: Exocrine and Endocrine Pancreas © OpenStax is licensed under a CC BY (Attribution) license
- Pancreas: Pancreas © OpenStax is licensed under a CC BY (Attribution) license
- Small Intestine © OpenStax is licensed under a CC BY (Attribution) license
- Layers of the Small Intestine: Histology of the Small Intestine © OpenStax is licensed under a CC BY (Attribution) license
- Layers of the Small Intestine: Transmission Electron Microscope Image © OpenStax is licensed under a CC BY (Attribution) license
- Circular Folds © علاء is licensed under a CC BY-SA (Attribution ShareAlike) license
- Segmentation © OpenStax is licensed under a CC BY (Attribution) license
- Plate of ʻOno Mango © Judgefloro is licensed under a Public Domain license
- Large Intestine © OpenStax is licensed under a CC BY (Attribution) license
- Histology of the Large Intestine © OpenStax is licensed under a CC BY (Attribution) license
- Honu_‘Iwalani Clayton_CCBY_2022 10 30 © ‘Iwalani Clayton is licensed under a CC BY (Attribution) license
- divider_maile
mid-portion of the stomach
continuous muscular digestive tube that extends from the mouth to the anus
includes teeth, tongue, salivary glands, gallbladder, liver, and pancreas
(also, buccal cavity) mouth
innermost lining of the alimentary canal
layer of dense connective tissue in the alimentary canal wall that binds the overlying mucosa to the underlying muscularis
muscle (skeletal or smooth) layer of the alimentary canal wall
Membrane that covers organs and reduces friction; also referred to as serous membrane.
portion of the pharynx flanked by the nasopharynx, oral cavity, and laryngopharynx that is a passageway for both air and food
muscular tube that runs from the pharynx to the stomach
alimentary canal organ that contributes to chemical and mechanical digestion of food from the esophagus before releasing it, as chyme, to the small intestine
terminal portion of the alimentary canal
passage of digested products from the intestinal lumen through mucosal cells and into the bloodstream or lacteals
section of the alimentary canal where most digestion and absorption occurs
(plexus of Meissner) nerve supply that regulates activity of glands and smooth muscle
(plexus of Auerbach) major nerve supply to alimentary canal wall; controls motility
region of the conducting zone that forms a tube of skeletal muscle lined with respiratory epithelium; located between the nasal conchae and the esophagus and trachea
part of the large intestine between the sigmoid colon and anal canal
muscular contractions and relaxations that propel food through the GI tract
voluntary process of swallowing and the involuntary process of peristalsis that moves food through the digestive tract
located posterior to the peritoneum
organ with both exocrine and endocrine functions located posterior to the stomach that is important for digestion and the regulation of blood glucose
first part of the small intestine, which starts at the pyloric sphincter and ends at the jejunum
part of the large intestine between the cecum and the rectum
taking food into the GI tract through the mouth
enzymatic breakdown of food
elimination of undigested substances from the body in the form of feces
aqueous solution of proteins and ions secreted into the mouth by the salivary glands
digestive enzyme from glands in the tongue that acts on triglycerides
accessory digestive organ of the mouth, the bulk of which is composed of skeletal muscle
mass of chewed food
chewing, mixing, and segmentation that prepares food for chemical digestion
chewing
soupy liquid created when food is mixed with digestive juices
alternating contractions and relaxations of non-adjacent segments of the intestine that move food forward and backward, breaking it apart and mixing it with digestive juices
lymphatic capillaries of the gut that absorb bile to form chyle
semisolid waste product of digestion
peptide hormone secreted in response to stomach distention that stimulates the release of hydrochloric acid
gastric gland cell that secretes hydrochloric acid and intrinsic factor
alkaline solution produced by the liver and important for the emulsification of lipids
largest gland in the body whose main digestive function is the production of bile
accessory digestive organ that stores and concentrates bile
process by which mixing waves gradually cause the release of chyme into the duodenum
movement of food through the GI tract
an exocrine gland that secretes a digestive fluid called saliva
gum
digestive enzyme in saliva that acts on starch
covering of the dentin of the crown of a tooth
portion of tooth visible superior to the gum line
bone-like tissue immediately deep to the enamel of the crown or cementum of the root of a tooth
region of the external nose between the eyebrows
deepest portion of a tooth, containing nerve endings and blood vessels
tooth used for crushing and grinding food
(also, canine) pointed tooth used for tearing and shredding food
midline, chisel-shaped tooth used for cutting into food
mucous membrane fold that attaches the bottom of the tongue to the floor of the mouth
skeletal muscle sphincter that regulates food movement from the pharynx to the esophagus
portion of the pharynx bordered by the oropharynx superiorly and esophagus and trachea inferiorly; serves as a route for both air and food
three-stage process of swallowing
smooth muscle sphincter that regulates food movement from the esophagus to the stomach
(also, cardiac region) part of the stomach surrounding the cardiac orifice (esophageal hiatus)
glycoprotein required for vitamin B12 absorption in the small intestine
dome-shaped region of the stomach above and to the left of the cardia
lower, funnel-shaped part of the stomach that is continuous with the duodenum
sphincter that controls stomach emptying
fold of alimentary canal mucosa and submucosa in the empty stomach and other organs
narrow channel formed by the epithelial lining of the stomach mucosa
gland in the stomach mucosal epithelium that produces gastric juice
gastric gland cell that secretes pepsinogen
gastrin-secreting enteroendocrine cell
digestive acid secreted by parietal cells in the stomach
inactive form of pepsin
gastric gland cell that releases hormones
(also, reflex phase) initial phase of gastric secretion that occurs before food enters the stomach
phase of gastric secretion that begins when food enters the stomach
artery that supplies oxygenated blood to the liver
vein that supplies deoxygenated nutrient-rich blood to the liver
vein that receives blood from hepatic sinusoids
drains systemic blood from the liver and flows into the inferior vena cava
hexagonal-shaped structure composed of hepatocytes that radiate outward from a central vein
major functional cells of the liver
yellowish bile pigment produced when iron is removed from heme and is further broken down into waste products
enzyme secreted by the pancreas that participates in lipid digestion
recycling mechanism that conserves bile salts
duct through which bile drains and enters the gallbladder
(also, sphincter of Oddi) sphincter regulating the flow of bile and pancreatic juice into the duodenum
structure formed by the union of the common hepatic duct and the gallbladder’s cystic duct
secretion of the pancreas containing digestive enzymes and bicarbonate
middle part of the small intestine between the duodenum and the ileum
end of the small intestine between the jejunum and the large intestine
pouch forming the beginning of the large intestine
(also, plica circulare) deep fold in the mucosa and submucosa of the small intestine
projection of the mucosa of the small intestine
small projection of the plasma membrane of the absorptive cells of the small intestinal mucosa
fuzzy appearance of the small intestinal mucosa created by microvilli
brush border enzyme that breaks down maltose and maltotriose into two and three molecules of glucose, respectively
brush border enzyme that breaks down lactose into glucose and galactose
brush border enzyme that breaks down sucrose into glucose and fructose
(also, crypt of Lieberkühn) gland in the small intestinal mucosa that secretes intestinal juice
mixture of water and mucus that helps absorb nutrients from chyme
(also, duct of Wirsung) duct through which pancreatic juice drains from the pancreas
(also, ampulla of Vater) bulb-like point in the wall of the duodenum where the bile duct and main pancreatic duct unite
point at which the hepatopancreatic ampulla opens into the duodenum
(also, Brunner’s gland) mucous-secreting gland in the duodenal submucosa
form of peristalsis in the small intestine
bacteria in the large intestine
small sac of fat-filled visceral peritoneum attached to teniae coli
small pouch in the colon created by tonic contractions of teniae coli
final segment of the large intestine
(vermiform appendix) coiled tube attached to the cecum
mesentery of the appendix
first region of the colon
(also, hepatic flexure) point, at the inferior surface of the liver, where the ascending colon turns abruptly to the left
part of the colon between the ascending colon and the descending colon
(also, splenic flexure) point where the transverse colon curves below the inferior end of the spleen
part of the colon between the transverse colon and the sigmoid colon
end portion of the colon, which terminates at the rectum
one of three transverse folds in the rectum where feces is separated from flatus
involuntary smooth muscle sphincter in the anal canal
voluntary skeletal muscle sphincter in the anal canal
long, slow, peristaltic wave in the large intestine
sphincter located where the small intestine joins with the large intestine
slow segmentation in the large intestine
propulsive movement in the colon activated by the presence of food in the stomach
anaerobic decomposition of carbohydrates
gas in the intestine

